News from WholeBlue Living - June 2019
If you’ve been wondering what I’ve been up to (as in, why no newsletter for more than a month) click on the video link above. It should explain it all. But if you want more, please read the story.
On late March of 2018, our niece gave birth to a healthy baby boy named Jayden. During his first year of life we watched as she struggled to parent. We did what we could to support her, including taking him for a few days at a time during the year. It turned out my sister (“nana”) ended up doing most of the work, a situation that wasn’t sustainable long term, for several good reasons. Although our niece wants to be mom, she continues to struggle to do the work.
As a result, on April 18 of this year, we have taken temporary legal guardianship of Jayden, giving our niece time to work out the struggles she has had so she can be a better parent.
As those of you who are parents understand, parenting is a lot of work. Most parents have nine months or so to prepare. We had half a day. So it has taken some time to build up a new routine and figure out where WholeBlue fits in. News may be a little sporadic in the next couple months but I continue to be committed to providing everything I promised to each of you.
Meanwhile, I’d love your support. If you’ve parented, please send me an idea for getting a 14-month old child to eat solid food!
News from WholeBlue Living - February 2019

What part do your genes play in cancer?
According to a study published in Pharmaceutical Research, “Only 5 percent to 10 percent of all cancer cases can be attributed to genetic defects, whereas the remaining 90 percent to 95 percent have their roots in the environment and lifestyle.”1
The lifestyle factors evaluated included: cigarette smoking, diet, alcohol, sun exposure, stress, physical inactivity and a few others. The authors noted that of all cancer-related deaths, “almost 25 percent to 30 percent are due to tobacco, as many as 30 percent to 35 percent are linked to diet, about 15 percent to 20 percent are due to infections. The remaining percentage are due to other factors.”
This suggests if you eat a healthy diet and you don’t smoke, you may cut your risk of getting cancer by more than half. The researchers said, “cancer prevention requires smoking cessation, increased ingestion of fruits and vegetables, moderate use of alcohol, caloric restriction, exercise, avoidance of direct exposure to sunlight, minimal meat consumption, use of whole grains, use of vaccinations, and regular check-ups.”
In addition to these changes, the researchers explored the role of inflammation and provided “evidence that cancer is a preventable disease that requires major lifestyle changes.”
The thing about cancer, however, is that you want to avoid it, not wait until you get it to try to treat it. There are a lot of reasons for this, especially the fact that in the United States “the overall contribution of curative and adjuvant cytotoxic chemotherapy to 5-year survival in adults was estimated to be 2.1 percent.”2
Yes, you read that correctly.
Most people who undergo the rigors of chemotherapy don’t survive beyond five years. The statistics include some cancers where five-year survival is much greater, such as some pediatric cancers and Hodgkin’s disease. Other cancers weren’t as survivable.
(Please note, these were patients who underwent chemotherapy, not all patients who got cancer. Some cancer cases do not require chemotherapy.)
The researchers noted, “a healthy lifestyle can nip [cancer] in the bud, whereas early diagnosis and treatment…doesn’t change the number of people getting cancer in the first place.
There are a few things you can do today to help prevent cancer in your body. First, eat plant-based foods. The consumption of animal-based foods has been historically “associated with increased cancer risk while [certain plant-based food components have been] associated with decreasing risk.”
This means, don’t just avoid foods with cancer-promoting factors, but eat foods with active cancer-suppressing mechanisms, such as every kind of fruit and vegetable as well as whole grains.
Also, as the researchers noted, cancer prevention means no more cigarettes, moderate alcohol use, exercise, avoiding direct sunlight exposure, getting vaccinated, and getting regular check-ups. And when you eat like this, you’ll be avoiding a lot more than cancer (as though that weren’t enough). Plant-based diets also help to minimize the risk (and sometimes reverse) other diseases such as heart disease, strokes, arthritis, and diabetes.
References
- Anand P, Kunnumakkara AB, Sundaram C, et al. Cancer is a preventable disease that requires major lifestyle changes. Pharm Res. 2008 Sep;25(9):2097-116. doi: 10.1007/s11095-008-9661-9. Epub 2008 Jul 15.
- Morgan G, Ward R, Barton M. The contribution of cytotoxic chemotherapy to 5-year survival in adult malignancies. Clin Oncol (R Coll Radiol). 2004 Dec;16(8):549-60.
News from WholeBlue Living - January 2019
What do you know about cholesterol?
Before I get to the answer for the latest WholeBlue quiz question, which was “Which of the following food contributes the most cholesterol to the typical American diet?” let’s talk about why cholesterol is important.
The American Heart Association says, “Cholesterol can join with other substances to form a thick, hard deposit on the inside of the arteries. This can narrow the arteries and make them less flexible – a condition known as atherosclerosis. If a blood clot forms and blocks one of these narrowed arteries, a heart attack or stroke can result.”1
There is also a potential link between cholesterol and some forms of cancer, Alzheimer’s and other diseases. For these reasons and more, lowering cholesterol is a good thing. To do that well, we need to know what raises or lowers our cholesterol levels.
First, the answer to the quiz question. The answer is eggs, which contribute about 24.6 percent of the cholesterol found in the typical American diet. Next is chicken at 12.5 percent (which answers the question, which comes first, the chicken or the egg). Then beef at 11 percent and cheese at 4.2 percent.
A single egg provides 212 mg of cholesterol. As mentioned in the moderation article, your body makes all the cholesterol you need so you really don’t need any in your diet. However, some dietary guidelines do set a number at less than 300 milligrams of cholesterol per day.
Let’s see how the cholesterol adds up for the average diet.
The USDA “Choose My Plate” guidelines recommend 5 to 6.5 ounces of proteins such as meat, poultry or fish every day. (They also include nuts, seeds and legumes in this category, so the protein does not need to be animal-based; however the typical American diet is based on animal protein.) Three ounces of boneless, skinless chicken breast provide 48 mg of cholesterol. Three ounces of roast beef provide 45 mg of cholesterol and other meats are comparable.
So if you stick to these guidelines and eat just under 7 ounces of any of these foods (except the eggs), you’ll stay under 300 mg. So far, so good.
The scientific research tells us why this matters. For example, vascular risk factors, such as high cholesterol, can be thought of as a ticking time bomb for Alzheimer’s disease. What’s bad for the heart may be bad for the mind.2
However, all of these foods also come with saturated fat. If you eat the amount of protein recommended by the guidelines through eating meat, you may not exceed the cholesterol amounts, but you will definitely exceed the saturated fat amount.
In addition, most of us don’t stop at the recommended amounts. These are:
1 small steak (eye of round, filet) = 3 ½ to 4 ounce-equivalents
1 small lean hamburger = 2 to 3 ounce-equivalents
1 small chicken breast half = 3 ounce-equivalents
½ Cornish game hen = 4 ounce-equivalents
1 can of tuna, drained = 3 to 4 ounce-equivalents
1 salmon steak = 4 to 6 ounce-equivalents
And remember, dairy, like cheese, falls under a different category from protein, but adds cholesterol and saturated fat.
It’s an interesting dilemma in that we can feel safe to eat the animal-based protein from a cholesterol perspective (based on dietary guidelines, and if we avoid eggs) but that same amount provides more saturated fat than we need (the safe level is none).
The American Heart Association recommends eating “no more than 6 percent of saturated fat as part of total daily calories for those who need lower cholesterol.” That’s about 120 calories for someone who should consume 2,000 calories a day to maintain their weight, equal to about 11 to 13 grams of saturated fat.1
Saturated fat primarily comes from animal products, however a few plant foods contain saturated fat, including coconut, coconut oil, palm oil and cocoa butter.
So the question is whether a person can keep daily intakes of saturated fat under 11 grams and cholesterol low. That answer is likely no, considering the following sources and amounts of saturated fat:
• Plain, low-fat yogurt (8 oz), 2.3 grams
• Plain, whole-milk yogurt (8 oz), 4.8 grams
• One egg, 1.6 grams
• One teaspoon butter, 2.4 grams
• One teaspoon coconut oil, 4 grams
• One grilled (no oil), boneless, skinless chicken breast .8 grams
• Sharp cheddar cheese (1 oz) 5 grams
• 1/4 cup coconut milk, 10 grams
• Boneless lamb (3 oz) 7.5 grams
• One slice bacon, 1 gram
• Burger King bacon and cheddar BK toppers 11 grams
• One Krispy Kreme original glazed doughnut, 5 grams
• One Pepperidge Farm soft-baked sugar cookie, 2.5 grams
• McDonald’s Southwestern Salad, 3 grams
While oils (except coconut oil) don’t contribute saturated fat, they aren’t much better for our bodies. A study published in Nutrition, Metabolism and Cardiovascular Diseases in 2007 found that all oils have a damaging effect on endothelial function after each meal, independent of what type of oil, or whether the oil was fresh, or deep fried.3
The endothelial is the lining of the heart and blood vessels. Loss of proper endothelial function can lead to cardiovascular disease. The oils studied included olive, soybean and palm.
The good news is people can lower their cholesterol 5 to 10 percent by cutting down on fatty meat, dairy and eggs, or lower it 10 to 15 percent on a vegetarian or flexitarian diet, or lower it 15 to 25 percent on a standard vegan diet.
But to really lower cholesterol levels, and nearly eliminate saturated fat—in a matter of weeks—eat a plant-based diet, which could lower cholesterol up to 35 percent. In addition, a plant-based diet also improves insulin sensitivity better than a conventional diabetic diet and can lead to a significant drop in LDL cholesterol, thereby reducing the risk of heart disease.4
References
- American Heart Association.
- Nutrition Facts
- Rueda-Clausen CF1, Silva FA, Lindarte MA, Villa-Roel C, Gomez E, Gutierrez R, Cure-Cure C, López-Jaramillo P. Olive, soybean and palm oils intake have a similar acute detrimental effect over the endothelial function in healthy young subjects. Nutr Metab Cardiovasc Dis. 2007 Jan;17(1):50-7. Epub 2006 Mar 20.
- Kahleova H, Matoulek M, Malinska H, et al. Vegetarian diet improves insulin resistance and oxidative stress markers more than conventional diet in subjects with type 2 diabetes. Diabet. Med. 2011;28(5):549–59.
News from WholeBlue Living - October 2018

Are you dying from frying?
I was recently reminded of why I eat plant based and why eating out is sometimes a very bad idea. It all started with a birthday gift from my husband of no cooking or meal planning for two days. Instead, Dennis took me to vegan restaurants around Denver. No work. Just great eating.
Unfortunately, eating at a vegan restaurant isn’t necessarily better than eating at a meat-based restaurant. The meals are often prepared with large amounts of fat and sodium, as well as processed food.
We thought it might be fun nonetheless. But, the fun stopped with our last meal.
Around 2008, I began to experience random but increasingly more common allergic responses. They’d start with redness and puffiness on my face and spread into a rash that sometimes spreads down my body. I’ve been working with an allergist, but so far we have been unsuccessful at figuring out the actual cause, but the most likely is food.
Since going plant-based, the number of attacks have significantly decreased. In fact, it has been nearly two years since my last attack. When I do have trouble, I have oral steroids (and an Epi-Pen, which thank God I’ve never had to use) available to take. I had mostly forgotten an attack was a possibility.
Until that last restaurant meal. As I ate, my face grew hot and began puffing up. I downed the first of my steroids and within about 30 minutes, it began to calm down.
But now I’m left wondering what happened. I called the restaurant for an ingredient list and the only thing different from what I would prepare is the fat. The meal contained a lot more fried food than I’m used to eating. (I’m used to eating none.)
That it might be the fat, makes sense. In a recent series of blog posts I wrote, “researchers found that “a high-fat diet may contribute to chronic inflammatory diseases of the airway and lung.”
My allergist said sometimes you just never know. It could even be a combination of things that causes the attacks. For example, one of his patients only reacts when she eats shrimp and then exercises. Otherwise shrimp is without problem.
One thing I do know is with all the extra oil I ate for my birthday weekend, my body was clearly inflammed. The conditions were right for a problem.
Everyone’s body gets inflammed on a high-fat, high-processed-food diet. (Remember, oil is a processed food.) My body just seems to externalize it more. At the same time, “a diet low in processed food can decrease inflammation.”
If your face swelled up for a week after eating too much fat, would you still do it? It’s one of the many reasons I keep trying to eat clean.
What’s your incentive?
Relax!
Stress is a component of nearly every mental, physical and spiritual health problem, either directly or indirectly causing it, or making it worse.
Relaxation can work like a medicine, if taken correctly, to reduce stress and mitigate its potential risks. It is a state of well-being where you are managing stress or anxiety; you feel calm. The more relaxed you are, the greater the benefits. It
- reduces stress and the symptoms of mental health conditions like depression, anxiety and schizophrenia
- lowers anger and frustration levels
- boosts confidence
- improves concentration and mood
- lowers heart rate, blood pressure and breathing rates
- reduces muscle tension and chronic pain
- reduces fatigue
We probably all know some techniques to help us relax. Let’s run through them. They can include:
- praying or meditating
- exercising
- reading
- watching a movie
- taking a bath
- breathing deeply
- painting or other creative process
- listening to music
- imagining you are somewhere peaceful
Nearly all of us know which of those relaxation techniques, or others, will help to calm us.
What’s more difficult for most of us, is remembering to practice them.
One way you can remember is to build in time to relax every time you transition to a new task. Here are five ideas.
- Before you start your next task, or at least every 45 minutes, devote 2 to 5 minutes to practicing a relaxation technique. Set a timer if you need the help.
- Whenever you come home, spend at least 5 minutes to transition. Either sit quietly in your favorite spot, lay down, or enjoy a cup of tea or coffee.
- Within 10 minutes of waking up every morning, spend 10 to 20 minutes praying, thanking God or meditating, depending on your spiritual perspective.
- Get yourself ready for the next day, by laying out clothes, making lunch, whatever you need first thing in the morning, and making a list of the top things (no more than 5) you need to accomplish. Once that’s done, spend 15 to 30 minutes reading or bathing or doing whatever soothes you to prepare you for sleep.
- Take time to stretch. Do some simple stretches at least 5 minutes a day, either to start your day, in the evening as you wind down, or as part of a transition.
Remember, to fully relax you need to stay away from technology, like cell phones or tablets. And please note, that some people, especially those who have serious psychological issues, may feel emotional discomfort with some relaxation techniques. If this happens to you, stop what you’re doing and talk to your mental health provider.
For more information on relaxation, check out one of the resources below.
https://www.healthdirect.gov.au/relaxation
http://www.mentalhealthy.co.uk/lifestyle/relaxation
https://www.mind.org.uk/information-support/tips-for-everyday-living/relaxation/
https://nccih.nih.gov/health/stress/relaxation.htm
https://www.helpguide.org/articles/stress/relaxation-techniques-for-stress-relief.htm
https://www.mentalhealthamerica.net/conditions/rest-relaxation-and-exercise
https://www.mayoclinic.org/healthy-lifestyle/stress-management/in-depth/relaxation-technique/art-20045368?pg=2

News from WholeBlue Living - September 2018
Healing mouthwash
According to Reviews.com, “The best mouthwash should wipe out bacteria, strengthen tooth enamel, and improve gum health.”
We might add, and not damage DNA. In a 2008 study evaluating the safety of dental products such as chlorhexidine-containing mouthwashes, genetic, or DNA damage was detected in the 13 study volunteers individuals who rinsed their mouths with it. The damage was not limited to cells in their mouths. After just a few weeks there was an increase in DNA damage in the cells lining their cheeks and in their peripheral blood cells.1,2
The good news is that it reduced plaque better than other antiseptic chemicals. However, there is more bad news. Not only do chlorhexidine-containing mouthwashes mess with DNA, but they also kill the essential natural flora on our tongues, and other things, such as nitrates. A 2008 study in Hypertension showed that “bacterial mediated conversion of nitrate to nitrite on the tongue could significantly increase nitrite in the plasma [blood] leading to…cardiovascular effects” such as lowered blood pressure and other benefits. The chlorhexidine swishes out these positive benefits.3,4
Until recently, chlorhexidine-containing mouthwashes were considered the “gold standard” in eliminating bacteria and improving gum health. However, there are other options, none of which cause DNA damage. In fact, they are health-promoting throughout the body.
For example, a study in the British Journal of Nutrition found that eating healthier led to better oral health. The 20 female study participants all had mild to moderate chronic periodontitis. After the guided nutritional study, the researchers measured significantly reduced pocket depth as well as lowered gingival inflammation, and levels of inflammatory cytokines, all of which are measures of periodontal health.5
The diet emphasized vegetables, fruits, whole grains, potatoes, beans, peas, lentils and spices. Water was the preferred beverage. As we’ve seen in numerous other research studies, such a whole-food, plant-based diet can lead to improvement of several health conditions including diabetes and heart disease.
In addition to a healthy diet, a 2011 study published in the International Journal of Dental Hygiene supports using green tea for its anti-bacterial and cavity-fighting properties.6
Green tea also helps boost immune function and fight some cancers, among other benefits.7,8
And green tea is better than the best mouthwash. A 2013 study compared chlorhexidine directly to green tea and found that the tea worked better at reducing plaque. It’s also less expensive, and as the other studies showed, safer.9
Adding amla powder (dried Indian gooseberry) to the tea, increases its cavity-stopping potential. The amla suppresses plaque formation(while the tea helps to kill off the bacteria).10 Amla also has shown to lower cholesterol.11
With all of the benefits of tea and amla on oral health and none of the side effects of chlorhexidine-containing mouthwashes, perhaps the next question is, where to find it. The best answer is to make your own.
For more information on the subject, check out what Michael Greger, M.D. at NutritionFacts.org says here. Or just cold-brew yourself some tea (let tea steep in tap water for two to four hours) add a little amla and store it in your refrigerator in a tightly sealed jar. Then just pour out what you need each day, swish and swallow (don’t spit).
References
- Ribeiro DA. Do endodontic compounds induce genetic damage? A comprehensive review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008 Feb;105(2):251-6. doi: 10.1016/j.tripleo.2007.07.045
- Eren K, Ozmeriç N, Sardaş S. Monitoring of buccal epithelial cells by alkaline comet assay (single cell gel electrophoresis technique) in cytogenetic evaluation of chlorhexidine. Clin Oral Investig. 2002 Sep;6(3):150-4. Epub 2002 Jul 25.
- Webb AJ, Patel N, Loukogeorgakis S, et al. Acute blood pressure lowering, vasoprotective, and antiplatelet properties of dietary nitrate via bioconversion to nitrite. Hypertension. 2008;51:784–790.
- Wink DA, Paolocci N. Mother was right: eat your vegetables and do not spit! When oral nitrate helps with high blood pressure. Hypertension. 2008 Mar;51(3):617-9. doi: 10.1161/HYPERTENSIONAHA.107.106617. Epub 2008 Feb 4.
- Jenzsch A, Eick S, Rassoul F, et al. Nutritional intervention in patients with periodontal disease: clinical, immunological and microbiological variables during 12 months. Br J Nutr. 2009 Mar;101(6):879-85. doi: 10.1017/S0007114508047776. Epub 2008 Aug 20.
- Awadalla HI, Ragab MH, Bassuoni MW, et al. A pilot study of the role of green tea use on oral health. Int J Dent Hyg. 2011 May;9(2):110-6.
- Benefits of green tea for boosting antiviral immune function. Michael Greger M.D. FACLM March 20th, 2017 Volume 3.
- Can green tea help treat cancer? Michael Greger M.D. FACLM March 6th, 2017 Volume 34.
- Balappanavar AY, Sardana V, Singh M. Comparison of the effectiveness of 0.5% tea, 2% neem and 0.2% chlorhexidine mouthwashes on oral health: a randomized control trial. Indian J Dent Res. 2013 Jan-Feb;24(1):26-34. doi: 10.4103/0970-9290.114933.
- Hasan S, Danishuddin M, Adil M, et al. Efficacy of E. officinalis on the cariogenic properties of streptococcus mutans: A novel and alternative approach to suppress quorum-sensing mechanism. PLOS Published: July 5, 2012.
- Amla vs. drugs for cholesterol, inflammation, & blood-thinning. Michael Greger M.D. FACLM October 30th, 2017 Volume 38.
News from WholeBlue Living - July 2018

No substitute for meat
The WholeBlue Living course has a lesson called, “Strange Foods” focused on some of the foods eaten by those following a whole-food, plant-based diet. They are strange only in that they are not typically seen in the standard American diet.
Many meat substitutes, are in this category. While meat substitutes are not typically part of a whole-food, plant-based lifestyle (because they are processed foods) they can be helpful with the transition, to fill cravings, or to add meatiness when cooking for meat eaters.
For example, sometimes I make a white bean chili that includes an option to add meatless sausage to it. When I make it for myself I don’t put in the sausage; however, when I make it for others, I do.
The problem with meat substitutes, however, is that they often don’t taste like the animal food they’re replacing. But even if they were an exact match, they aren’t the healthiest option. Most are high in fat and sodium, which create similar long-term health risks to meat consumption.
Some can even make you sick immediately. For example, Quorn brand products are made with mycoprotein, a fungi developed from vat-grown and fermented fusarium venenatum fungus that has been linked to severe allergic reactions.
If meat substitutes are a poor substitute, many would ask how someone on a plant-based diet gets protein. While this is a common question, it’s really the wrong question to ask. People who eat enough calories from a variety of healthy plant-based foods to sustain their ideal body weight, will automatically consume enough protein.
For example, the recommended dietary allowance (RDA) of protein for a woman is 46 grams. (This assumes the woman is neither pregnant nor lactating.) That woman could get nearly double that amount of protein—83 grams—by eating the following plant-based food.
For breakfast: polenta with blueberries, pumpkin seeds and flax along with a slice of whole grain bread with almond butter and half a grapefruit.
For lunch: lentil salad on greens with a no-oil dressing, a slice of whole-grain bread and a pear.
For dinner: whole grain pasta topped with tomato sauce, and cannellini beans, accompanied by a tossed green salad, cooked broccoli and an apple.
Some believe that plant protein is inferior to animal protein, but this idea is not true. It came from studies performed on rodents more than a 100 years ago.
It is true that some plant proteins are relatively low in certain essential amino acids. But the American Heart Association and other expert organizations agree that, “Plant proteins can provide all the essential amino acids.” Our bodies maintain free amino acid reserves to ensure we always have the right balance. Therefore, it is nearly impossible to design a diet of whole plant foods that is sufficient in calories, but deficient in protein. (Note it must be “sufficient in calories” you do have to eat enough, and those calories should be healthy options.)
Some would argue that meat is even more efficient at providing protein because there is so much per serving, especially if it’s “high quality” meat such as organic, free-range or grass-fed. But while such meats may contain fewer contaminants, the fact remains that in numerous studies, animal protein has been linked to kidney problems, heart disease, diabetes and much more.
If you want to avoid the health risks that often come with consuming animal-derived foods, you need to avoid the food itself, regardless of how “high quality” its source is.
The focus on protein is misguided. Deficiency in the United States is rare. In fact, most individuals consume more protein than they need every day. Even vegetarians and vegans get 70 percent more protein than they need every day.1
Meat substitutes can help you enjoy your favorite “meaty” meals as you transition to a whole-food, plant-based diet, or to fill cravings in slightly healthier ways, but they are not needed to meet protein requirements. Meals that include legumes, whole grains and fruits and vegetables will provide a variety of nutrients, including protein, and are all you need.
However, if you still want a meat substitute, consider minimally processed foods such as tofu, tempeh and seitan. Or, if you really want an animal-derived food like cheese or meat to fill a craving, allow yourself to indulge in the real thing a couple times a year.
But if you feel the need to eat it more often, reconsider your goals for eating plant-based.
Reference
1. Rizzo NS, Jaceldo-Siegl K, Sabate J, Fraser GE. Nutrient profiles of vegetarian and nonvegetarian dietary patterns. J Acad Nutr Diet. 2013 Dec;113(12):1610-9. doi: 10.1016/j.jand.2013.06.349. Epub 2013 Aug 27.
WholeBlue Living's Defining Facts - June 2018
Erectile dysfunction may signal early death
The quiz question this month was: “What percent of U.S. men over the age of 40 have erectile dysfunction?” And the answer is, 40 percent of men over 40” have erectile dysfunction. While that’s interesting, what is more informative is the correlation between erectile problems and heart disease.
According to researchers, “new erectile dysfunction in men aged 40 to 49 years was associated with a 50-fold increase in the incidence of coronary artery disease,” that is, heart disease, including sudden death.
It turns out that erectile dysfunction and our top killer, coronary artery disease, are just two ways the same disease manifests. Whether in the penis or heart, arteries damaged from atherosclerosis look the same—inflamed, clogged and crippled.
Atherosclerosis is a systemic disorder that uniformly affects all major blood vessels in the body. Stiffened arteries can’t relax, open wide and let the blood flow normally. In fact, in two-thirds of men arriving at emergency departments with crushing chest pain for the first time, their penis had been trying to warn them that something was wrong for years.2
The problem often shows up first in the penis because the penile arteries are half the size of the arteries in the heart. This means a man wouldn’t necessarily feel the buildup of plaque in the heart arteries when that same amount of buildup could nearly clog the penile artery, resulting in impotence. Plaque is the buildup of fatty deposits in our arteries.
The connection between erectile dysfunction and heart disease is clear. In fact, research has shown that blood flow in a man’s penis is a great predictor of his cardiac stress test’s results. The accuracy of such a test is 80 percent.3
Nearly 30 million men in the U.S. and approximately 100 million men worldwide have erectile dysfunction. This means that the United States has up to 30 percent of the impotence, even though fewer than 8 percent of the world’s population lives in the United States. What makes the United States No. 1 with this issue? Likely, our diets.
While drugs like Viagra treat the symptom, they mask the underlying problem—unhealthy arteries. On the other hand, a whole-food, plant-based diet will help attack the root causes, including cholesterol, oxidation, and inflammation—with no bad side effects.4,5,6
Even men younger than 40 should care, because high cholesterol levels and other indicators of heart disease predict erectile dysfunction—and therefore the potential of heart attacks, strokes and shortened lifespans. There is no amount of Viagra that will help a man’s sex life after a fatal heart attack or crippling stroke.7
References
- Inman BA, Sauver JL, Jacobson DJ, et al. A population-based, longitudinal study of erectile dysfunction and future coronary artery disease. Mayo Clin Proc. 2009 Feb;84(2):108-13.
- Montorsi F, Briganti A, Salonia A, et al. Erectile dysfunction prevalence, time of onset and association with risk factors in 300 consecutive patients with acute chest pain and angiographically documented coronary artery disease. Eur Urol. 2003 Sep;44(3):360-4; discussion 364-5.
- Corona G, Fagioli G, Mannucci E, et al. Penile doppler ultrasound in patients with erectile dysfunction (ED): role of peak systolic velocity measured in the flaccid state in predicting arteriogenic ED and silent coronary artery disease. J Sex Med. 2008 Nov;5(11):2623-34. Epub 2008 Sep 8.
- Esposito K, Ciotola M, Giugliano F, et al. Mediterranean diet improves erectile function in subjects with the metabolic syndrome. Int J Impot Res. 2006 Jul-Aug;18(4):405-10. Epub 2006 Jan 5.
- King DE, Egan BM, Geesey ME. Relation of dietary fat and fiber to elevation of C-reactive protein. Am J Cardiol. 2003 Dec 1;92(11):1335-9.
- Wang F, Dai S, Wang M, Morrison H. Erectile dysfunction and fruit/vegetable consumption among diabetic Canadian men. Urology. 2013 Dec;82(6):1330-5.
- Chung SD, Chen YK, Lin HC, Lin HC. Increased risk of stroke among men with erectile dysfunction: a nationwide population-based study. J Sex Med. 2011 Jan;8(1):240-6. Epub 2010 Aug 16.


Calorie targets
If you follow Michael Greger’s Daily Dozen* here are some calorie ranges to help you out, assuming you eat only the minimum servings.
Vegetables, including greens and cruciferous: 150 calories
Fruits, including berries: 300 calories
Whole grains: 300-400 calories
Beans and legumes: 300-400 calories
Flax seeds: 70 calories
Nuts and seeds: 200 calories
Spices: 10 calories
Total Calories: 1,330 to 1,530
To calculate the total calories of your favorite foods, click here for a calorie counter.
________________________________
*To download the Daily Dozen app, go here for the Google Play store or here for iTunes.
Weight gain on a plant-based diet
Most people who start a whole-food, plant-based diet lose weight, even without trying. However, it is possible to unintentionally gain weight on a plant-based diet, especially if your calorie requirements are low. This could happen, for example, with someone who must eat fewer than 1,500 calories a day to lose weight. (To find out your ideal weight click here. )
Many in the plant-based community promote eating until satiation, which essentially means eat when you’re hungry and stop when you’re full. It’s simple enough advice, but there are a few glitches to that formula.
For people whose caloric requirements are smaller than average or people who don’t have a “stop” signal in their stomachs, gaining weight on a whole-food, plant-based diet is possible.
If you fit one of those exceptions, or worry that you do, the following tips will help keep you on track with your weight goals as you transition to a whole-food, plant-based diet.
Find a satiety “indicator”. Some people can’t easily gauge satiety; they feel either hungry or stuffed, but never just “comfortably full.” These people can’t rely on their stomachs to tell them to stop eating to avoid weight gain. If you fall into this category, there are a couple of things you can do.
First, you can stop eating when you’re only 80 percent full. That is, when you think you may still be a little hungry if you stop eating. This is a common method to avoid overeating used through the regions of the world where the longest-living people reside.
The option is to plan your meals in advance to make sure you know how much you can eat without overdoing it, and to check for hidden or unexpected calories. (See following items.)
Avoid processed foods. Some people gain weight on a plant-based diet because they add too many processed foods, including breads, pastas, refined sugars and oils. This category also includes prepared foods such as veggie burgers, other meat replacements, TVP (textured vegetable protein), and other “fake” meat and dairy foods. While technically a whole-food, plant-based diet shouldn’t include any processed foods, including vegan “fake” foods, most of us fall prey to this one.
And it doesn’t take much. For example, a tablespoon of oil in a salad dressing adds 124 empty calories. If you’re trying to eat fewer than 1,500 calories, that oil is around 10 percent of your total for the day.
Worse, the oil not only provides no nutrition, but can lead to inflammation in your body. Same thing for sugar, whether in the form of honey or brown sugar or agave nectar. Two tablespoons of sugar is equal to 100 calories.
Adding two pieces of bread to your day adds around 200 calories, and while healthier than oil or sugar, its more refined. A better option when you’re trying to lose weight is to eat your grains in the most whole form possible. This way you’ll get the same calories, but it will be harder to overeat.
Identify “hidden” calories. While a smoothie is a great way to add fruits and greens to your diets, it’s also a great way to over-consume calories. For example, a smoothie with a banana, a half-cup of strawberries, a cup of greens and a cup of soy milk is close to 300 calories. Add any nut butter, avocado or liquid sweetener like maple syrup and the calories can double or go even higher.
If you’re going to include smoothies, make sure the calorie count is low or you’re truly drinking it in place of other meal items.
Expect initial water weight. A newly adopted whole-food, plant-based diet often means a steep increase in the amount of dietary fiber consumed. As a result, your body may hold a little more water weight, but it doesn’t mean you have any more fat. The good news is, if you encounter this problem it will resolve within weeks.
In addition, a plant-based diet includes more water naturally, through the higher water content of plants. In a sense, it means you’re re-hydrating, which is a good thing. Again, it will resolve itself.
Being proactive
In addition to identifying the potential pitfalls in advance, it’s good to also plan your meals, or at least food categories, to ensure you have a good variety of foods that stay within your calorie goals.
- Eat more low-calorie vegetables.
Most vegetables are lower in calories, especially the healthiest vegetables such as green leafy vegetables and cruciferous vegetables like cauliflower, broccoli and Brussels sprouts. Other lower-calorie vegetables include summer squash, tomatoes, cucumbers.
A good rule of thumb to remember if you’re trying to keep it low, is to think leafy, watery or crunchy. If the vegetable is smooth and creamy (or could be made that way) like potatoes and winter squash, it’s more likely to be higher in calories.
- Keep your grains whole and your servings small.
Most whole grains contain 100 to 150 calories per ½ cup serving. A serving of bread or other refined grains has a similar amount of calories but is easier to overeat. If you’re trying to lose or maintain weight, it’s best to eat no more than the minimum three servings per day, and keep them whole.
- Fresh fruit is best.
In general, the denser the fruit the greater the calories. Fruits like apples, pears and bananas are about 100 calories each. Whereas juicier fruits like watermelon, oranges and pineapple have only about 50 to 75 calories per serving. Berries are generally in this category, as well. Dried fruit is the most calorie dense and should be avoided if you’re trying to lose weight.
- Drink water.
If you’re trying to keep your calories to a minimum, your best beverages are water, unsweetened teas or coffee (without cream or sugar). Everything else just adds calories without nutrients (and in some cases does harm).
- Mind your beans.
Legumes, peas and soy are healthy options for a whole-food, plant-based diet, but keep in mind they contain about 110 calories per half-cup serving. If you’re trying to lose weight, keep your servings to no more than three per day.
- Nuts, seeds and more.
It’s easy to overdo with nuts and seeds. Heart healthy flax seeds contain 70 calories per the recommended two tablespoons and walnuts 200 calories per the suggested quarter cup per day. If you’re going to skimp in this category, it’s best to eat the walnuts or other nuts only a couple times a week and keep the flax in.
- Plan ahead
If you’re trying to lose weight, planning is key. You especially want to pay attention to total calories and portion sizes. Eating out is another area where the calories add up quickly. For example, restaurant food is often higher in fat, due to added oils.
Whatever your situation, the key is to enjoy your food and to feel like you have enough. This is important because eating plant-based should be a lifestyle, not a short-term diet, so you can live your most whole life every day.
Remember, a 1,500-calorie, whole-food, plant-based diet is packed with much more life-saving nutrition than one filled with processed foods, dairy and meat.
Finally, if you’re struggling to lose weight, give it time. The weight didn’t add up fast, and will be unlikely to decrease fast.
WholeBlue Living's Defining Facts - May 2018
Hard shell still a hard sell
Last month we looked at the health benefits and drawbacks of eating fish. Someone asked whether the same holds true for shellfish. Given that fin fish, what we covered in the last issue, and shellfish are not related, this article will explore the benefits and drawbacks of eating shellfish.
Fin fish, like salmon and trout, are cold-blooded vertebrate animals with fins and gills that live in water. Shellfish are aquatic invertebrates with shells. They can be divided into two additional categories: crustacea, such as shrimp, crab and lobster; and mollusks, such as clams, mussels, oysters, calamari and scallops.
Nutritionally, fish and shellfish are similar when it comes to protein, cholesterol and calories. For example, clams and lobster contain around the same amount of protein as salmon. However, clams are slightly lower in protein and octopus has considerably more than other fish and shellfish.
Clams, crab, mussels and oysters may actually help to lower cholesterol because they contain sterols, which interfere with the absorption of cholesterol, while shrimp and calamari may have the opposite effect. But in general, the cholesterol benefits (or not) are similar to fin fish.1
Shellfish do have a few nutritional outliers. For example, per 100 grams, oysters contain the most zinc of any other food. Clams are high in iron and vitamin B12. And crustaceans supply high amounts of choline, which accelerates the synthesis of acetylcholine, a neurotransmitter important in memory and muscle control.
At the same time, shellfish are not generally a good source of omega-3s, the primary health benefit connected to fish.2
Shellfish from the crustacea category leads to the most allergic reactions from any type of fish. These allergies tend to be severe. About 60 percent of people with shellfish allergy experience their first reaction as adults. The allergy never goes away. The good news is you can be allergic to one and not the other, because fin fish and shellfish are not related.
This also means being allergic to one type does not always mean that you must avoid both. However, there can be overlap between a crustacea and mollusk allergy. People who are allergic to one type of shellfish are generally advised to avoid them all.
In addition to the higher incidence of allergy to shellfish, toxins also can be a problem, just as with fin fish. For example, dinoflagellates, the reddish-brown organisms responsible for “red tides,” make a toxin that collects in several species, including clams, crabs, mussels and scallops. Shellfish contaminated with these organisms are unsafe.
Other types of shellfish poisoning include paralytic, neurotoxic and amnesic poisoning. Unfortunately, the substances that cause some of these, including ciguatera and scombroid poisonings, are heat stable. This means no matter how properly you handle or cook the contaminated shellfish, you will become sick.
Symptoms depend on the specific type of poisoning. With ciguatera poisoning, the poisonous ingredient is ciguatoxin. This poison is made in small amounts by certain algae and algae-like organisms called dinoflagellates.
Symptoms of ciguatera poisoning occur about two to 12 hours after eating the fish and include abdominal cramps, severe diarrhea, and nausea and vomiting. After the initial symptoms, sufferers experience additional strange sensations such as a feeling that their teeth are about to fall out, headache or a metallic taste in their mouths. The symptoms often are worsened by alcohol consumption.
Ciguatera poisoning is not limited to shellfish, however. Small fish that eat the algae also can become contaminated. If larger fish eat a lot of the smaller, contaminated fish, the poison can build up to dangerous levels and sicken a person. In addition, according to a 2007 report from North Carolina, the ciguatera toxin itself can be sexually transmitted from a fish-eater to a non-fish-eater.3
Scombroid poisoning is another fish-related disease not limited to shellfish. With scombroid, the poisonous ingredient is a combination of histamine and other similar substances. After the fish dies, bacteria create large amounts of the toxin if the fish is not immediately refrigerated or frozen. Unfortunately, “the appearance, taste and smell of the fish are poor guides as to the presence of histamine.”4
Symptoms most often occur immediately after consuming the poisoned fish and include: breathing problems, hives and itching, nausea and vomiting, and a peppery or bitter taste. While these symptoms are similar to an allergic reaction, scombroid poisoning is not an allergy.
As discussed last month, mercury and other toxic chemicals are present in all fish, including shellfish. According to the U.S. Environmental Protection Agency, “One of the primary risks of consumption of contaminated fish and shellfish is exposure to methyl mercury [which comes] almost exclusively through the consumption of fish and shellfish.”5
Finally, there is a possibility that eating fish that eat a type of blue-green algae could lead to the development of Lou Gehrig’s or Alzheimer’s disease in some people. Nearly all types of blue-green algae found all over the world, not just in the sea, produce a neurotoxin named BMAA for short. (Its long name is beta-N-methylamino-L-alanine.)
Researchers involved in a study published in the 2010 issue of Harmful Algae, said, “We examined several blooms of cyanobacteria in South Florida, and the BMAA content of resident animals, including species used as human food. A wide range of BMAA concentrations were found, ranging from below assay detection limits to…a concentration associated with a potential long-term human health hazard.”6
Other scientists looked at BMAA’s relationship to disease. “We hypothesize that individuals who develop neurodegenerations may have a genetic susceptibility because of inability to prevent BMAA accumulation in brain proteins and that the particular pattern of neurodegeneration that develops depends on the polygenic background of the individual.”7
Another study published in 2009 sought to clarify the issue. Those researchers looked at whether BMAA was likely to be present in people with Alzheimer’s disease (AD) or amyotrophic lateral sclerosis (ALS), otherwise known as Lou Gehrig’s disease. The researchers included controls in the study of those free from neurologic disease and those with a genetic condition. They concluded that “the occurrence of BMAA in North American ALS and AD patients suggests the possibility of a gene/environment interaction, with BMAA triggering neurodegeneration in vulnerable individuals.”8
This research indicates that, whether raw or cooked, seafood can be risky. A 2010 article in the journal of Clinical Microbiology on the epidemiology of seafood-associated infections sums it up. The authors noted that consumer awareness of the risk is important. In particular, “Persons with underlying medical conditions such as liver disease, diabetes, or immunosuppressing conditions are at higher risk of acquiring severe infection and should be especially careful.” The report concludes by saying, “Seafood is part of a healthful diet, but seafood consumption is not risk-free.”9
References
- Bonesmart.org.
- Foodallergy.org.
- Cluster of ciguatera fish poisoning–North Carolina, 2007. Centers for Disease Control and Prevention (CDC). MMWR Morb Mortal Wkly Rep. 2009 Mar 27;58(11):283-5.
- National Library of Medicine.
- NEPIS EPA
- Brand LE, Pablo J, Compton A, Hammerschlag N, Mash DC. Cyanobacterial Blooms and the Occurrence of the neurotoxin beta-N-methylamino-L-alanine (BMAA) in South Florida Aquatic Food Webs. Harmful Algae. 2010 Sep 1;9(6):620-635.
- Bradley WG, Mash DC. Beyond Guam: the cyanobacteria/BMAA hypothesis of the cause of ALS and other neurodegenerative diseases. Amyotroph Lateral Scler. 2009;10 Suppl 2:7-20.
- Pablo J, Banack SA, Cox PA, et al. Cyanobacterial neurotoxin BMAA in ALS and Alzheimer’s disease. Acta Neurol Scand. 2009 Oct;120(4):216-25.
- Iwamoto M, Ayers T, Mahon BE and Swerdlow DL. Epidemiology of Seafood-Associated Infections in the United States. Clin. Microbiol. Rev. April 2010 vol. 23 no. 2 399-411.


Emotions and asthma
The answer to the recent quiz question, “Exposure to which of the following could trigger an asthma attack in someone who suffers from the disease?” is all of the above, from this list that included dry wind, hormonal changes, a funny movie, and irritants in the environment.
Other asthma triggers include anger, fear, yelling, crying, depression, sulfites in foods, medical problems like reflux, and cold air. Doctors are clear about the triggers; they are numerous and varied. What isn’t clear about asthma is the cause.
For most people, asthma begins in childhood; however, it can develop at any point in life. It is a chronic lung disorder without a known cure, that causes swelling and inflammation in the lungs. It affects more than 25 million people in the United States, or about 8 percent of the population. More than a quarter of the sufferers are children.
Whether asthma begins in childhood or adulthood, the symptoms such as wheezing, coughing and chest pressure are the same, and the treatments similar, although children face different challenges.
According to the Asthma and Allergy Foundation of America, at least 30 percent of adult-onset cases are triggered by allergies; however, others put the estimate as high as 50 percent. Other triggers include environmental or workplace irritants, including smoking or secondhand smoke.
Environmental factors appear to play a large role in triggering asthma in children, as well, although most experts agree the triggers are not fully understood. Airway infections and genetics are other possible factors.
What researchers have established is a link between asthma and emotions, possibly as a cause, especially in young children. According to a 2016 article in Pediatrics, children in foster care are two to three times more likely to suffer from asthma.1
A 2009 study found that children raised with unusual amounts of stress and who lived in the presence of environmental risk factors such as pollution had an up to 50 percent increased risk of developing asthma. For example, the researchers found that children whose mothers smoked during pregnancy were more likely to develop asthma when their home environment was also stressful.2
While researchers won’t say stress causes asthma, the link is strong, especially for children. For adults, strong emotions—positive or negative—can cause existent asthma to flare. The reason appears to be related to how breathing changes—becoming quicker and shallower—when we feel strong emotions. For those whose airways are particularly sensitive, such changes can be enough to trigger an asthma attack. In addition, the effort it takes to cry, laugh, yell or even cough or sneeze can affect breathing and trigger symptoms.
In 2000, researchers at Stanford University studied both the emotional and physical response to stimuli among asthmatic and non-asthmatic patients. They found several important differences. The study, published in Psychosomatic Medicine, revealed that participants with asthma seemed to have reduced lung function when they experienced mood changes. The more negative the mood, the more severe the changes, although the variances were notable on both ends. These same responses didn’t seem to exist among people who weren’t afflicted with asthma.3
In an article published on WebMD, psychiatrist Glenda MacQueen discussed a study presented in 2001 at the annual meeting of the American Psychiatric Association. It looked at the connection between emotion and asthma. MacQueen evaluated 80 patients with mild to moderate asthma. First, she identified participants who were highly “suggestible,” that is, highly responsive to cues and suggestions in their environment.
MacQueen administered a placebo solution of salt water in the kind of inhaler typically used for asthma medications, to the nine people identified as suggestible and the eight identified as nonsuggestible. Prior to administration, she told the subjects the solution would cause their airways to constrict.
Even though the solution was harmless, because of MacQueen’s suggestion that it might cause harm, six of the patients—including five from the “suggestible” group—experienced airway constriction.
What triggers emotional arousal is highly variable among us. MacQueen says what’s key is to “reflect on the emotional triggers—the settings and circumstances and the kinds of feelings associated with those situations—that seem to precede asthma attacks. Simply knowing what those situations are can lend people a sense of mastery over a condition that is often terrifying.”4
The relationship between asthma and emotion goes even deeper. Research has shown a strong link between asthma and major depressive disorder. The two problems share several risk factors and have similar patterns of dysregulation. Unfortunately, few studies have examined whether improving symptoms of depression also results in better asthma control or improved quality of life.5
Traditional Chinese medicine has always accepted the role of emotions in physical illness. In traditional Chinese medicine, every organ is correlated to an emotion and every organ has a partner organ. The belief is they work together to keep the body in balance.
In this tradition, the lungs are in partnership with the large intestine. The Chinese belief is that many breathing and bowel disorders are rooted in excess grief and sadness and that excessive grieving can lead to disorders of both the lungs and the large intestine.
Scientists have begun to discover the same thing. In her book, Molecules of Emotion, the late Candace Pert, a neuropharmacologist who worked at the National Institutes of Health and Georgetown University Medical Center, described how we store emotion and memory in all of our glands, organs, tissues and cells. She said, “Your body is your subconscious mind. [The] physical body can be changed by the emotions we experience.”
Not only are those energy charges stored in our physical body, as Pert described, but they also appear to be stored at an energetic level at places called alarm points or meridian points. We all have emotions and memories such as failure, disappointments, suffering or loss hidden away or suppressed in our bodies, to be retrieved, reformed, and released or ignored, and left to fester. Wounds that never heal.
Some who have sought to treat the underlying emotions—such as mind-body protocols aimed at healing emotions at this root level, appear to have had success. In her counseling practice, Chris Cline uses the Splankna protocol, a biblically based mind-body procedure, to alleviate the roots of emotional trauma. Part of the Splankna protocol is to “clear” emotions using the meridian points Pert describe.
Cline has seen firsthand the power of emotions on asthma and the ability of mind-body work to heal. “I was on oxygen for three years and in October 2017 I was healed. I haven’t been on oxygen since and I’m off my asthma medications.” Cline says she was healed by God through the Splankna protocol.
Another approach to improving asthma comes through breath training protocols, such as the Buteyko method. “This method is based on the assumption that numerous medical conditions, including asthma, are caused by chronically increased respiratory rate or deeper breathing (hyperventilation).”6
Many who adhere to the Buteyko method find relief from their asthma, although the mechanism can’t be clinically documented in all cases. Perhaps there is some link to the mechanisms found in the mind-body approaches.
While diet can also help improve asthma and allergy symptoms, the emotional connection appears to show the best promise for long-term, lasting improvement.
References
- Turney K, Wildeman C. Mental and Physical Health of Children in Foster Care. Pediatrics. October 2016.
- Islam T, Gauderman WJ, Berhane K, et al. Relationship between air pollution, lung function and asthma in adolescents. Thorax. 2007 Nov;62(11):957-63. Epub 2007 May 21.
- Ritz T, Steptoe A. Emotion and pulmonary function in asthma: reactivity in the field and relationship with laboratory induction of emotion. Psychosom Med. 2000 Nov-Dec;62(6):808-15.
- WebMD.
- Van Lieshout RJ, MacQueen G. Psychological Factors in Asthma. Allergy Asthma Clin Immunol. 2008; 4(1): 12–28. Published online 2008 Mar 15. doi: 10.1186/1710-1492-4-1-12.
- Wikipedia.
WholeBlue Living's Defining Facts - April 2018
Something’s fishy
The true or false quiz question a couple weeks ago, was, “Farmed fish has a lower level of contaminant (or no contaminants) compared to wild-caught fish.”
Before looking at the answer, it’s important to understand the bigger picture. It is certainly a well studied one.
In general, fish is a good food to eat. Unfortunately, we have ruined it. Even though we attach labels to fish like, “sustainable” or “wild-caught” or “farmed,” according to Amro Hamdoun, who studies ecological developmental biology at Scripps, “we still haven’t figured out how to address whether it’s contaminated or not.”
In a study reported in a 2016 issue of Peer J, researchers analyzed hundreds of peer-reviewed articles, studying older “legacy” chemicals, such as DDT and mercury, as well as newer industrial chemicals, such as flame retardants and coolants.1
The researchers found persistent organic pollutants (POPs) in fish in all of the world’s oceans; although the concentrations of such contaminants are highly variable, as much as 1,000-fold in one region or group of fish. The good news is there is a drop in contaminants by 15 percent to 30 percent per decade. Lead author Lindsay Bonito said, “This means that the typical fish that you consume today can have approximately 50 percent of … most POPs when compared to the same fish eaten by your parents at your age.”2
The Washington State Department of Health agrees that contaminant levels are falling. “The good news is both wild and farmed salmon have low levels of mercury, PCBs, and other contaminants.”3
The truth—and the reason the answer to the quiz question is false—is that we have polluted our lands and waterways so much, that no fish is immune to contamination. How such contaminants get into fish is not fully known, and removing the fat when cleaning or cooking does not seem to reduce the amount of the contaminants. Additionally, we have no way of telling which fish from which waters will have lower levels.
Most other states monitor fish contaminants, toos, and find similar problems. For example, in Minnesota, which has one of the most extensive fish monitoring programs in the United States, the primary contaminant of concern is mercury. Much of the mercury in those waters comes from the air as the result of emissions from coal combustion and mining, and other human sources.
Another major contaminant in that area is PCBs. A form of synthetic oils, PCBs were used in many applications such as electrical transformers, cutting oils, and carbonless paper. Although banned in 1976, they remain in the water and lake sediments, albeit at slowly decreasing levels.4
There are numerous other contaminants, each with their own health risks. They come from a variety of sources, including industrial and municipal discharges, agricultural practices, and stormwater runoff, as well as chemicals from the land or air being deposited through rainfall.
The contaminants build up in our bodies over time. For example, it can take five years or more for women in their childbearing years to rid their bodies of PCBs, and 12 to 18 months to significantly reduce mercury levels. Such accumulation may lead to health problems, from small, hard-to-detect changes to birth defects and cancer.5
Yet, consumption of small amounts of fish can be healthy long term. The Adventist Health Study 2, which has been following 96,000 Americans since 2002, found that the people who lived the longest were not vegans or meat-eaters. They are “pesco-vegetarians,” or pescatarians,” people who eat a plant-based diet that includes a small amount of fish.6
In other Blue Zone communities, small amounts of fish are commonly eaten on average two to three times a week, apparently not affecting longevity. (A small amount of fish is no more than 3 ounces before it is cooked, or about the size of a deck of cards.)
At the same time, there is a wide body of other research that indicates many ill effects from eating fish due to the contaminants. For example, a 2011 study published in the American Journal of Clinical Nutrition found that the consumption of fish like salmon, swordfish, bluefish, mackerel or sardines may increase our risk of atrial fibrillation—an irregular heartbeat rhythm associated with stroke, dementia, heart failure and a shortened life span.7
In addition, six separate meta-analyses each suggest that fish consumers tend to be at greater risk for type 2 diabetes. That data also indicate that the risk for diseases like diabetes is not connected to the fish itself, but to the primarily man-made industrial chemicals in the waters, all of which are highly resistant to breaking down in the environment.
For example, fish consumption has been shown to be associated with significant cognitive deficits due to small amounts of methylmercury, the most toxic form of mercury.8
Fish oil doesn’t seem to fare any better, even those that were purified did not effectively remove all the industrial contaminants.
What’s worse, put all the research together, including an analysis published in the Journal of the American Medical Association in 2013, and it turns out the omega-3s in fish and fish oil may offer no protective effects on lifespan, cardiac death, sudden death, heart attack or stroke.
Research does indicate, however, that fish can help with brain health. The results of a double-blind randomized interventional trial published in 2014 in Cerebral Cortex provided evidence that extra long-chain omega-3s “exert positive effects on brain functions in healthy older adults.”
But while fish has the preformed DHA and EPA evaluated in the research, it likely contains the various pollutants, as well. For those who decide to not eat fish, there is an option to get contaminant-free DHA/EPA from algae oil taken from sources outside the seas.
If you do want to eat fish and are wondering whether a fish is good for you, check out the U.S. Environmental Protection Agency’s fish advisories, located on its website, to determine which fish is fine for you.9
Note: Next issue we’ll cover shellfish, including shrimp.
References
- Bonito LT, Hamdoun A, Sandin SA. Evaluation of the global impacts of mitigation on persistent, bioaccumulative and toxic pollutants in marine fish. PeerJ. 2016 Jan 28;4:e1573.
- Study Finds Toxic Pollutants in Fish Across the World’s Oceans. Scripps.
- Washington state.
- Minnesota.
- Seafood.
- Conscious Lifestyle magazine.
- Shen J, Johnson VM, Sullivan LM, et al. Dietary factors and incident atrial fibrillation: the Framingham Heart Study. Am J Clin Nutr. 2011 Feb;93(2):261–6.
- Yokoo EM, Valente JG, Grattan L, et al. Low level methylmercury exposure affects neuropsychological function in adults. Environ Health. 2003 Jun 4;2(1):8.
- EPA.

The downside(s) of milk
Part 2 of 2
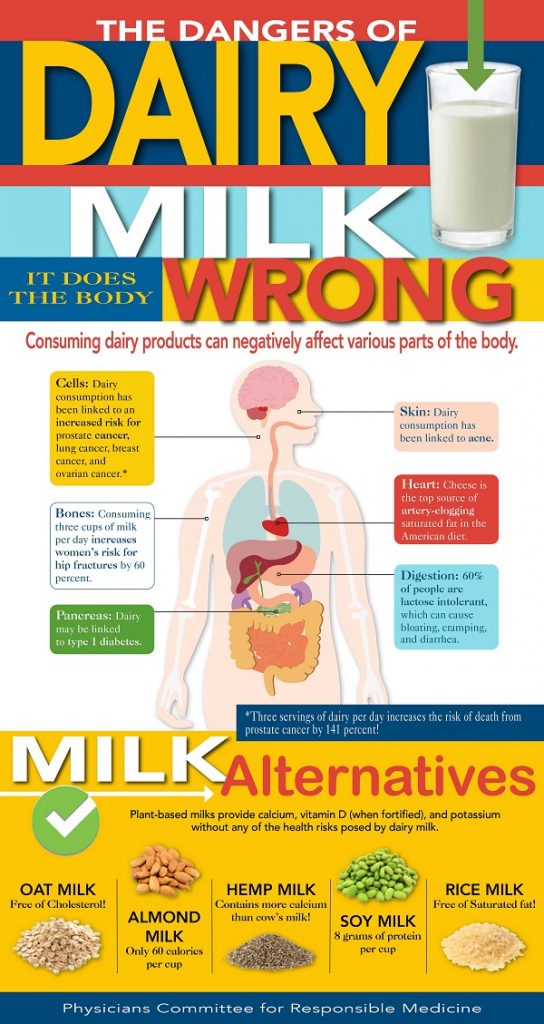
Part 1 of this article evaluated nine commonly promoted benefits to milk. Only one, its link to lowered diabetes risk, seems to be connected to the milk rather than the nutrients not unique to the milk. However, the health risks with milk may outweigh this benefit.
The chart illustrates just some of the dangers of dairy. We’re going to evaluate these, as well as a couple others.
The first is cancer. Dairy consumption has been linked to an increased risk for prostate cancer, lung cancer, breast cancer and ovarian cancer. In a study published online in the British Journal of Cancer, researchers followed 22,788 participants from Sweden who were lactose intolerant. As part of the study, they monitored the cancer rates for the participant’s immediate family members, as well.
The researchers found that the rates of lung, breast and ovarian cancers decreased for the lactose-intolerant study participants; however, those who included dairy—family members and the general Swedish population—did not experience the same reduction in cancer risk.1
A prospective study among 1,334 men with nonmetastatic prostate cancer, found that “whole milk consumption after prostate cancer diagnosis was associated with increased risk of recurrence, particularly among very overweight or obese men.”2
Next, while the dairy industry claims that milk helps strengthen teeth and bones, the claims appear to come more from calcium’s role, and the amount of calcium in milk, than the milk itself. In fact, research seems to demonstrate just the opposite. One such study found that consuming 3 cups of milk daily increases women’s risk for hip fractures by 60 percent.3
The investigators also found that a large amount of milk in a daily diet did appear to be linked to an increased risk of death in both men and women during the study period.
While the study evaluated in the last issue of Defining Facts indicated that high-fat milk was linked to a lower risk of type 2 diabetes; however, more than a dozen studies have been conducted that indicate that “early cow’s milk exposure” appears to “increase the risk” of type 1 diabetes by about 50 percent. The researchers are still investigating what about the milk is causing the problem.4
Acne is another problem linked to milk consumption. Research indicates that the same compound in milk that is linked to cancer is linked to acne.5
The Harvard Nurses’ Study, published in the Journal of the American Academy of Dermatology, found an association between milk intake during adolescence and severe physician-diagnosed teenage acne. The study, funded in part by the National Dairy Council, found an even greater connection for skim milk than for other forms of milk.6
Based on data from the Harvard School of Public Health, cheese is the top source of artery-cloggng fat in the American diet. Regular cheese contributes about 8.5 percent of American’s saturated fat intake, while pizza adds another 5.9 percent. While we can avoid saturated fat intake completely, since even plant-based foods have some, avoiding most animal products will lower our daily intake to acceptable levels.7
Saturated and trans fats contribute to the progression of several diseases, including autoimmune diseases, cancer and heart disease, and can also cause insulin resistance, the underlying cause of pre- and type 2 diabetes.
Milk and other dairy products are also a problem when it comes to digestion. Estimates range from 11 to 65 percent of people experience some form of lactose intolerance as they age. Lactose intolerance can cause bloating, cramping and diarrhea.
Research has also linked dairy to childhood constipation. A 2013 study found 100 percent improvement in constipation when children stopped consuming all dairy.8
Other studies from around the world found similar results, including a 1998 New England Journal of Medicine study where they concluded that “In young children, chronic constipation can be a manifestation of intolerance of cow’s milk.”9
In addition, milk is linked with an increased risk of Parkinson’s. A meta-analysis of that involved more than 300,000 people found a significantly increased risk of Parkinson’s disease with dairy consumption, including milk, cheese and yogurt. The researchers estimated that for every cup of milk or its equivalent consumed per day, Parkinson’s risk increased 17 percent.10
So where do you get your calcium if not from milk or dairy? It turns out, bone health is not just about calcium. Here are a couple more study results to help explain. A study in the 2006 American Journal of Clinical Nutrition found that “doubling the fruit intake is associated with a 5 percent higher spine mineralization” and that eating lots of fruit in childhood may be protective.11
So fruit is one answer. And the following study adds legumes and vegetables, as well. The Singapore Chinese Health Study, published in the 2014 Journal of Nutrition, found that a “diet rich in plant-based foods, namely vegetables, fruits, and beans, such as soy, may reduce the risk of hip fracture.”12
But it’s not just important to grow bone (i.e., spine mineralization). It’s also important to stop bone loss. It is thought that excessive free radicals may contribute to bone loss. The assumption is that fruits help to increase bone building cells, and decrease bone-eating cells, tipping the balance toward greater bone mass. Now the short definition of free radicals is that they are thought to be responsible for aging and tissue damage in our bodies.
Interestingly, this study focused on prunes, or dried plums. So if you’re interested in replicating the effects, you may want to stock up on prunes.13
In fact, taking calcium can actually be harmful. In fact, the government no longer recommends that we supplement, since calcium supplements can increase the risk of heart attacks. In addition, the recommend daily intake appears to be higher than is actually needed for most people.
The bottom line is a plant-based diet that provides the amount of calories you need to maintain your optimal weight should provide everything you need for optimal bone and teeth health.
References
- Ji J, Sundquist J, Sundquist K. Lactose intolerance and risk of lung, breast and ovarian cancers: aetiological clues from a population-based study in Sweden. Br J Cancer. Published online October 14, 2014.
- Tat D, Kenfield SA, Cowan JE, et al. Milk and other dairy foods in relation to prostate cancer recurrence: Data from the cancer of the prostate strategic urologic research endeavor (CaPSURE™). Prostate. 2018 Jan;78(1):32-39.
- Michaëlsson K, Wolk A, Langenskiöld S, et al. Milk intake and risk of mortality and fractures in women and men: cohort studies. BMJ. 2014 Oct 28;349:g6015.
- Gerstein HC. Cow’s milk exposure and type I diabetes mellitus. A critical overview of the clinical literature. Diabetes Care. 1994 Jan;17(1):13-9.
- Acne, dairy and cancer: The 5alpha-P link. Danby FW. Dermatoendocrinol. 2009 Jan;1(1):12-6.
- Adebamowo CA, Spiegelman D, Danby FW, et al. High school dietary dairy intake and teenage acne. J Am Acad Dermatol. 2005 Feb;52(2):207-14.
- National Cancer Institute. Risk Factor Monitoring and Methods: Table 1. Top Food Sources of Saturated Fata among U.S. Population, 2005–2006. NHANES.
- Crowley ET, Williams LT, Roberts TK, et al. Does Milk Cause Constipation? A Crossover Dietary Trial. Nutrients 2013, 5(1), 253–266.
- Iacono G1, Cavataio F, Montalto G, et al. Intolerance of cow’s milk and chronic constipation in children. N Engl J Med. 1998 Oct 15;339(16):1100–4.
- Jiang W, Ju C, Jiang H, Zhang D. Dairy foods intake and risk of Parkinson’s disease: a dose-response meta-analysis of prospective cohort studies. Eur J Epidemiol. 2014 Sep;29(9):613-9.
- Lanham-New SA. Fruit and vegetables: the unexpected natural answer to the question of osteoporosis prevention? Am J Clin Nutr. 2006 Jun;83(6):1254–5.
- Dai Z, Butler LM, van Dam RM, et al. Adherence to a vegetable-fruit-soy dietary pattern or the Alternative Healthy Eating Index is associated with lower hip fracture risk among Singapore Chinese. J Nutr. 2014 Apr;144(4):511-8.
- Hooshmand S, Arjmandi BH. Viewpoint: dried plum, an emerging functional food that may effectively improve bone health. Ageing Res Rev. 2009 Apr;8(2):122–7.
WholeBlue Living's Defining Facts - March 2018
Health-promoting fats
A couple weeks ago I asked the multiple-choice question, Which fat is health-promoting? The choices were: 1. Extra-virgin olive oil; 2. Coconut oil; 3. Safflower oil; 4. Both 1 and 2; 5. None of the above.
If you read the January issue of Defining Facts, the answer should have been easy. But if you got it wrong, it’s understandable. There is a lot of confusion about fats and oils in the popular media today.
The answer to the question is No. 5, None of the above.
The truth is, “all oils, including olive oil, have been shown to cause a constant and significant decrease in endothelial function after meals.”1
Remember, the endothelium is the lining of the blood vessels in our bodies. People who have poor endothelial function, that is an endothelium that is inflamed or otherwise injured, are at greater risk for heart disease and more.
Some research does indicate that a diet that includes olive oil, such as the Mediterranean diet, is healthier for the heart than the standard American diet. Let’s look at that statement, though.
First, note the comparison. The standard American diet, that is the diet most Americans eat regularly, is high in meat, dairy and other high-fat foods, and low in fruits, vegetables and whole grains.
The Mediterranean diet is essentially the opposite of this. Research has consistently shown that a diet higher in fruits and vegetables and whole grains, and lower in animal protein and high-fat foods, contributes to health.2
For example, the Bill & Melinda Gates Foundation-funded 2010 Global Burden of Disease Study analyzed risk factors for death and disease and determined that in the United States, the worst aspect of our diet is lack of fruit. And that’s just the top of the list.
The other flaw is the assumption that the health improvements seen in the Mediterranean diet over the standard American diet were due to the olive oil. In fact, many researchers suggest that the diet was healthier despite the olive oil.
The truth is, the more oil we consume, in any form, the more we damage the endothelium.3
Research shows that extra-virgin olive oil is somewhat protective, but that was compared to butter.4
However, all oils, including olive oil, have been shown to cause a constant and significant decrease in endothelial function after meals. This includes coconut oil, another popularly promoted oil. It is being marketed as an almost cure-all with antimicrobial, cancer-fighting, heart-disease-reducing, Alzheimer’s-curing health benefits. But the research does not bear this out.
Some doctors says to look at the health on some tropical islands, where they eat a lot of coconut. For example, there was an apparent absence of stroke and heart disease on the island of Kativa. But it turns out their diets centered around tubers (like sweet potatoes), with fruits, greens, nuts, corn and beans. They did eat meat a few times a week, but overall, they ate a whole-food, plant-based diet. In addition, they ate the whole coconut, not simply the oil.
We covered coconut in more detail in the January issue of Defining Facts, so check it out below for more details.
The bottom line is oils are processed foods, and consumption of oil should be avoided whenever possible. If you do want to use olive oil, mixed with equal parts of vinegar, it works great as a furniture polish. And coconut oil may be better served on our skin.
That said, if you must use a little oil, and that’s the only thing keeping you on a healthier whole-food, plant-based diet, just limit it as much as possible.
References
- Forks Over Knives.
- de Lorgeril M1, Salen P, Martin JL, Monjaud I, Delaye J, Mamelle N. Mediterranean diet, traditional risk factors, and the rate of cardiovascular complications after myocardial infarction: final report of the Lyon Diet Heart Study. Circulation. 1999 Feb 16;99(6):779-85.
Rueda-Clausen CF1, Silva FA, Lindarte MA, Villa-Roel C, Gomez E, Gutierrez R, Cure-Cure C, López-Jaramillo P. Olive, soybean and palm oils intake have a similar acute detrimental effect over the endothelial function in healthy young subjects. Nutr Metab Cardiovasc Dis. 2007 Jan;17(1):50-7. Epub 2006 Mar 20. - Tentolouris N1, Arapostathi C, Perrea D, Kyriaki D, Revenas C, Katsilambros N. Differential effects of two isoenergetic meals rich in saturated or monounsaturated fat on endothelial function in subjects with type 2 diabetes. Diabetes Care. 2008 Dec;31(12):2276-8. doi: 10.2337/dc08-0924. Epub 2008 Oct 3.


Milk is the wagame
(Part 1 of 2)
When I was in my early 20s I worked as a nanny, caring for a 3-year-old girl. One day we heard her singing, “Milk is the wagame.” Or at least that’s what we thought she said.
It turns out she was really attempting to sing “Milk is the one for me.” She had picked up the line, and the catchy tune, from a television commercial that was popular at the time. From that point forward, I used her line and sang, “milk is the wagame” whenever the tune ran through my mind.
Today I think this confusing word is more appropriate when it comes to milk. The milk industry says milk is good for us. We hear “milk is the one for me” but the truth is, milk is the wagame.
Search for the “health benefits of milk” and you will find several themes promoted repeatedly. Search for harms of milk and you will find an equal number of problems. In this part I’ll cover the purported benefits, and in Part 2, I’ll cover the harms.
A recent internet search on the benefits brought up the following themes:
- Nourishes the skin
- Re-hydrates the body
- Provides relief from acidity
- Improves vitamin and mineral intake, including calcium
- Lowers diabetes risk
- Reduces risk of cardiovascular disease
- Helps develop and maintain healthy bones and teeth
- Aids in weight loss
- Rebuilds muscles
Let’s take them one at a time. First, the claim that milk nourishes the skin. This claim has to do with applying milk topically, that is directly on the skin.
Lactic acid acts as an exfoliant, and enzymes in the milk help to smooth skin. And studies have demonstrated that a 12 percent lactic acid cream works to smooth and tone skin. As a result, some therapeutic skin creams contain lactic acid.1
But that’s topically applied. What happens if you drink it? The next claim is that milk re-hydrates the body. This just means it provides some of the fluid or water that our bodies need every day. If you don’t have access to water, milk may be a better choice, but water is more direct. This claim seems to be a stretch. Just drink water.
The next claim is that milk provides relief from acidity, otherwise called heartburn. The truth is that milk can actually increase heartburn symptoms; however, it is not always the case with low-fat milk. Rather than trying to figure out if milk will work, a better option for occasional tummy upset, including bloating, is carbonated water (but not soda).2,3
The next claim is that milk improves vitamin and mineral intake, including calcium. One site makes the claim, “A person who consumes a carton of whole milk doubles his chances of fulfilling his calcium requirement for the day…. Calcium, along with all of the other essential minerals listed above [Vitamins A and B12, D, carbohydrates, phosphorous, selenium, magnesium, protein, zinc, and riboflavin], are necessary for the daily diet in order to ensure proper functioning of every aspect of our body.”4
The authors imply that milk is the only way we can get these nutrients, or that milk supplies them at ideal levels not found in other foods. Neither of those ideas is true. Of all the nutrients, calcium is the most linked with milk. It is true that milk has calcium. However, as described in Part 2 of this article, milk may not be the best source of calcium. We’ll get to that in a moment.
The next claim, lowers diabetes risk, sounds significant. And, in fact, at least two studies seem to substantiate that claim. One study, published in 2016, found that people who had higher concentrations of dairy fat in their blood seemed to have lower diabetes rates.5
The other study, presented at the 2014 annual meeting of the European Association for the Study of Diabetes (EASD) in Vienna, Austria, included data for nearly 27,000 people (60 percent women), age 45–74 years, culled from the Swedish Malmö Diet and Cancer Study. Study participants were tracked for 14 years after original data collection.6
The researchers found that study participants eating eight portions of high-fat dairy a day (including cream and whole milk) had a 23 percent lower incidence of developing diabetes than those eating one portion a day. The same effect was not found for those eating low-fat dairy products.
(By the way, the study also looked at diabetes rates connected to eating meat and meat products like sausage, and found an increased risk of developing diabetes.)
Lead study author Dr. Ulrika Ericson said, “Our observations may contribute to clarifying previous findings regarding dietary fats and their food sources in relation to Type 2 diabetes. The decreased risk at high intakes of high-fat dairy products, but not of low-fat dairy products, indicate that dairy fat, at least partly, explains observed protective associations between dairy intake and Type 2 diabetes.”
The “eight portions” of high-fat dairy in the study were the equivalent of eight servings of about 6 ounces of whole milk or a little over 1 ounce of whole cream per day, or about 2½ tablespoons of cream each.
Should you add full-fat dairy to your diet? Read on so you may compare the risks and make a fully informed decision.
The next claim is that milk reduces the risk of cardiovascular disease. That also sounds very promising, but it doesn’t appear to be true. A 2016 study by Harvard Chan School researchers published in The American Journal of Clinical Nutrition looked at the relationship between dairy fat intake and risk of cardiovascular diseases, such as heart disease and stroke.7
The researchers followed more than 43,000 men from the Health Professionals Follow-Up Study, 87,000 women in the Nurses’ Health Study, and 90,000 women in the Nurses’ Health Study II. After adjusting for smoking, physical activity and other factors known to influence the development of heart disease, researchers found that dairy foods, including full-fat dairy milk, yogurt, butter, cheeses and cream, were not found to increase heart disease risk. But this was compared to a typical American diet that contains high amounts of refined carbohydrates and sugars.
So from where does the claim come? It is made based on research on calcium itself, just not, it appears, the calcium from milk. (Again, I’ll cover calcium in Part 2)
Another claim, and in fact the one we seem to hear the most often, is that milk helps to develop and maintain healthy bones and teeth. Again, this claim is based on the calcium in milk. It is true that calcium is essential for the growth and proper development of a strong bone structure. However, getting calcium from milk may not be the best option. We’ll cover that in Part 2.
The next claim is that milk aids in weight management. An article in the 2006 issue of the American Journal of Clinical Nutrition found some evidence of a link between some full-fat dairy and weight maintenance, however the findings were only in certain groups and only for some dairy products.8
The link does not appear to be strong for milk per se, but rather studies seem to suggest a link between calcium and weight maintenance as well as better weight maintenance when dairy is consumed “while on a reduced-calorie diet.”
The final claim is that milk rebuilds muscle. A 2007 study seems to support this claim. The study, published in the American Journal of Clinical Nutrition, compared cow milk to soy milk and a carbohydrate drink, and found that cow milk drinkers gained more muscle. The study was funded by the National Dairy Council.9
The full results include that “the consumption of either milk or soy protein with resistance training promotes muscle mass maintenance and gains” and that “the measured essential amino acid content of both proteins was not significantly different.”
Of the nine claims, only two can be attributed to milk, and only one of those is related to a disease, the claim that it lowers diabetes risk, and then only at small amounts.
In Part 2 of this article, I’ll look at the other side, the health problems researchers have identified connected to milk, as well as ways to get calcium into your diet.
References
- Walter P Smith, PhD. Epidermal and dermal effects of topical lactic acid. JAAD. Sept. 1996. Volume 35, Issue 3, Part 1, Pages 388–391.
- Feldman M, Barnett C. Relationships between the acidity and osmolality of popular beverages and reported postprandial heartburn. Gastroenterology. 1995 Jan;108(1):125-31.
- NutritionFacts.org. Club soda for constipation.
- Organic Facts.
- Mohammad Y. Yakoob, Peilin Shi, Walter C. Willett, Kathryn M. Rexrode, Hannia Campos, E. John Orav, Frank B. Hu, Dariush Mozaffarian. Circulating Biomarkers of Dairy Fat and Risk of Incident Diabetes Mellitus Among US Men and Women in Two Large Prospective Cohorts. Circulation. 2016; CIRCULATIONAHA.115.018410. Originally published March 22, 2016.
- Swedish National Data Service.
- Mu Chen Yanping Li Qi Sun An Pan JoAnn E Manson Kathryn M Rexrode Walter C Willett Eric B Rimm Frank B Hu. Dairy fat and risk of cardiovascular disease in 3 cohorts of US adults. The American Journal of Clinical Nutrition, Volume 104, Issue 5, 1 November 2016, Pages 1209–1217, Published: 24 August 2016
- Magdalena Rosell Niclas N Håkansson Alicja Wolk. Association between dairy food consumption and weight change over 9 y in 19,352 perimenopausal women. The American Journal of Clinical Nutrition, Volume 84, Issue 6, 1 December 2006, Pages 1481–1488.
- Healthy Eating.
WholeBlue Living's Defining Facts - February 2018
Chocolate is good for you!
It seems like every February we hear the news that chocolate is good for us. There is a lot of truth to that. But before you go out and buy a Hershey bar, read on. Not all chocolate is beneficial, nor is it good for you in all of its forms.
Let’s get the bad out of the way first. The fat, sugar and excess calories are the bad side of chocolate. In addition, milk, if the chocolate contains it, can be problematic. According to the authors of a study published in 2007 in the journal Circulation, “The antioxidant effect of cocoa is potentially [weakened] in the [blood] if the chocolate is ingested as milk chocolate or in combination with milk.”1
What’s left?
What’s left when you take fat, sugar and milk out of chocolate is the cocoa. According to the authors of that same study in Circulation,“Natural cocoa powder can be [considered] a health food.”1
Chocolate is made from the usually roasted and ground seeds of the Theobroma cacao tree. Theobroma is the Greek term for “food of the gods.” In Aztec society, one of the first to revere chocolate, chocolate was reserved for priests, warriors and nobility. It was not until 1876 that milk, cocoa powder and cocoa butter were combined to form what we now know as chocolate.
Benefits of chocolate
Cocoa powder offers the health benefits of chocolate without the fat, sugar and milk. Although it isn’t as tasty, there are many ways to make it tasty and get all the benefits.
The health benefits of cocoa powder include improved coronary artery function, which is the blood delivery system for your body. When this system is working well, our bodies receive a continuous supply of the oxygen and nutrients we need to stay healthy and function normally.
Chocolate can improve the function of coronary arteries in the heart within two hours of consumption.1
Improvement in artery function with chocolate extends to our peripheral arteries. Study participants with peripheral artery disease, or blockage in the arteries feeding our limbs, could walk about a dozen more yards two hours after eating dark chocolate than they could before the chocolate.
Research indicates that chocolate can also reduce our stroke risk. Study findings published in the journal Neurology in 2012 suggest that “moderate chocolate consumption may lower the risk of stroke.”2
A Newsweek article references yet another heart-related benefit. “Eating chocolate could help prevent atrial fibrillation—a condition that causes an irregular heartbeat.”
Published in the medical journal Heart, the study found that adults who ate chocolate up to three times a month were up to 20 percent less likely to suffer from atrial fibrillation than those who had chocolate once a month or less.3
How much is too much?
Many of the compounds in chocolate that contribute to its pleasure would be psychoactive if they were able to get into our brains in large quantities. According to a 2010 article in Psychology Today, these compounds are the reason so many people love chocolate and the same reason that “for a small percentage of the population, eating chocolate can produce rage, paranoia and anger that occur without warning.”4
One of these compounds, phenethylamine (PEA), is a molecule that resembles amphetamine and other psychoactive stimulants. However, when we eat chocolate, PEA is rapidly metabolized by another enzyme known as MAO, and about 50 percent of it is gone within 10 minutes.
Chocolate also contains small amounts of the amino acid tyramine, which can powerfully induce the release of adrenaline, increase blood pressure and heart rate, and produce nausea and headaches. Tyramine is also metabolized by MAO; however, its metabolism may be slowed by the simultaneous metabolizing of PEA.
According to the author of the Psychology Today article, Gary L. Wenk PhD, the consequence of having both of these chemicals “hang around too long in the body would be high blood pressure, a fast beating heart, heightened arousal, racing thoughts, anger, anxiety and rage,” leaving some people vulnerable “to experience significant shifts in mood after eating chocolates with high cocoa powder levels.”
Chocolate also contains a small amount of the marijuana-like neurotransmitter called anandamide. This molecule can easily cross the blood-brain barrier; however, according to Wenk, “the levels in chocolate are probably too low to produce an effect on our mood by itself.”
Chocolate also contains many healthful substances such as magnesium salts. This means that your chocolate craving may actually be a nutrient deficiency. In a blog post by one of her patients, medicinal herbalist Daniela Turley makes that claim. “First there is a sugar-craving element and second the chocolate component,” she said. “There may be a nutrient that is in chocolate that the body is craving.”5
Some say the missing nutrient is magnesium. The good news is you don’t need to take a supplement to find out. In addition to chocolate, great sources of magnesium include dark leafy greens such as spinach, Swiss chard, kale, or collard greens; seeds like pumpkin seeds and flax seeds; all kinds of nuts; beans and legumes such as lentils and chickpeas; and fruits like bananas, strawberries, grapefruit, figs and avocado.
Whether you want chocolate because your body needs to replace a missing nutrient or you just need to feel happier, don’t let anyone tell you any differently. According to the American Dietetic Association, “Chocolate cravings are real.”6
References
- Circulation. 2007 Nov 20;116(21):2376-82. Epub 2007 Nov 5.
- Neurology. 2012 Sep 18;79(12):1223-9. Epub 2012 Aug 29.
- Newsweek.
- Psychology Today.
- Stylecaster blog post.
- J Am Diet Assoc. 1999;99: 1249–1256.

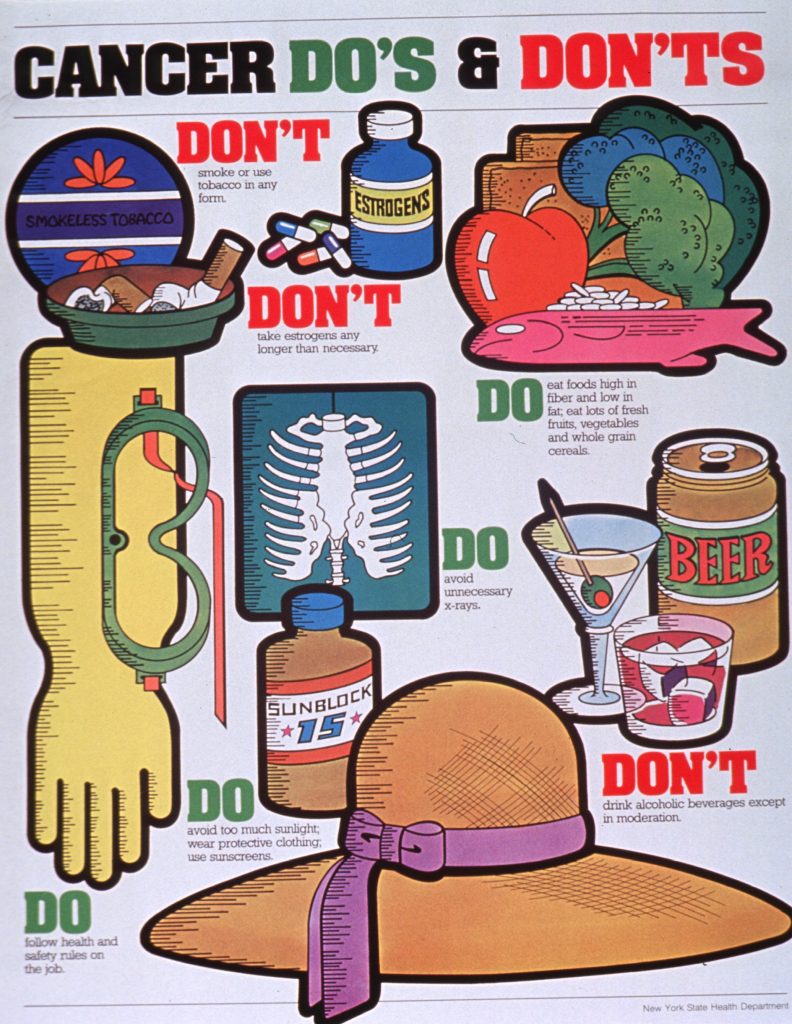
Avoiding cancer
When you visit the dentist every six months, whether you know it or not, your dentist generally performs a cancer screening, merely by looking for abnormalities in your mouth. If the dentist finds something suspicious, patients are referred to the next level of care. Screening for most other cancers often is not that simple, but the goal is the same, to detect cancer before symptoms appear. Cancer that is caught early is often easier to treat or cure.
While screening seems like a great idea, not all screening tests are helpful. And doctors often don’t tell their patients that most screening tests have risks, some of which can cause serious problems. Cancer screening may involve blood or urine tests or even medical imaging such as mammography.
According to the National Cancer Institute, some screening procedures can cause bleeding or other problems. For example, colon cancer screening done through colonoscopy can cause tears in the lining of the colon.
In addition, false-positive test results can be a concern. This is when results appear abnormal even though there is no cancer. Such a result is usually followed by more tests and procedures, which also have risks, and can cause a lot of anxiety that may last for years.
False-negative test results are also possible. This is when the test results appear normal even though there actually is cancer. Someone who receives such a result may delay seeking medical care.
Also, detecting some cancers early may not improve a person’s health or help that person to live longer. In some cases, the cancer would never cause symptoms or become life-threatening. In other cases, finding and treating the cancer early does not improve the chance of a cure or extend life. And treatments for cancer have side effects, many of them nasty.
Is screening beneficial?
Since for some cancers, screening is unequivocally the best path, and in others it likely won’t extend life and could even be harmful, how do we know what to do? Doctors will offer their opinions, but the ultimate decision for or against screening must be made by each person, based on the best available evidence. And because doctors often don’t provide what is needed, patients should seek the evidence for themselves.
The Agency for Healthcare Research and Quality (AHRQ) offers a list of clinical guidelines and recommendations for screening and treating a large variety of diseases, including cancer. It is an excellent place to start for information on weighing the options.
The U.S. Preventive Services Task Force (USPSTF), is one resource listed on the AHRQ site. Created in 1984, the USPSTF is an independent group of national experts in prevention and evidence-based medicine who work to improve the health of all Americans by making evidence-based recommendations about clinical preventive services such as screenings, counseling services or preventive medications.
Following are the USPSTF’s recommendations for three common cancers: colorectal, breast and prostate. The recommendations are quite different from each other, but with the exception of breast cancer, are commonly accepted by most physicians. (For more information on why breast cancer is different, check out the video series on this topic at NutritionFacts.org.)
For breast cancer screening the USPSTF recommends:
- Individualized decision to begin biennial screening according to the patient’s circumstances and values for women age 40–49 years.
- Screening every two years for women age 50–74.
- No recommendations for women who are older than 75 years.
The USPSTF offers the following in its benefits and harms section:
- There is convincing evidence that screening with film mammography reduces breast cancer mortality, with a greater absolute reduction for women age 50 to 74 years than for younger women.
- Harms of screening include psychological harms, additional medical visits, imaging and biopsies in women without cancer, inconvenience due to false-positive screening results, harms of unnecessary treatment, and radiation exposure.
- False-positive results are a greater concern for younger women; treatment of cancer that would not become clinically apparent during a woman’s life (overdiagnosis) is an increasing problem as women age.
For colon cancer, the USPSTF recommends:
- Screening with one of three options: fecal occult blood testing (FOBT), sigmoidoscopy, or colonoscopy for adults age 50 to 75 years.
- No automatic screening for adults age 76 to 85. No screening for adults over age 85.
- The research indicates that the benefits of screening outweigh the potential harms for 50- to 75-year-olds.
For prostate cancer screening, the USPSTF does not recommend prostate-specific antigen (PSA)-based screening. It goes on to note: “There is convincing evidence that PSA-based screening programs result in the detection of many cases of asymptomatic prostate cancer, and that a substantial percentage of men who have asymptomatic cancer detected by PSA screening have a tumor that either will not progress or will progress so slowly that it would have remained asymptomatic for the man’s lifetime (i.e., PSA-based screening results in considerable overdiagnosis).”
When it comes to colorectal cancer screening, and possibly other screenings, the USPSTF information offers something most physicians do not. Options. The guidelines list three evidence-based options for screening for this often very treatable cancer. But most physicians only mention one, colonoscopy.
On its website the USPSTF cautions doctors to “practice shared decision making” and suggests that “discussions with patients should incorporate information on test quality and availability.” For patients who aren’t being invited into decision-making discussions about their own bodies, the AHRQ and USPSTF should help.
Whether or not you choose to get screened, it’s better to try to minimize your chances of getting cancer. Here are a few evidence-based options that could lower your risks.
- Eat more vegetables overall, but those that are particularly cancer fighting include garlic, bell peppers, broccoli, carrots, celery, green onions, mushrooms, spinach and other green leafy vegetables.
- Eat more fruit, making sure to include lots of berries.
- Avoid all meats, but especially processed meats like bacon and lunch meat.
- Eat more ground flax, which research has shown to be especially powerful against cancers like breast and prostate.
- Eat other seeds and nuts, such as sesame.
- Eat white button mushrooms, which may have a cancer preventive effect with regard to breast cancer development.1
- Eat more soy foods (unless you’re allergic to soy).
- Eat more beans and legumes, especially if you are at higher risk for colorectal cancer.
- Eat more whole grains.
- Avoid eggs. Harvard University researchers followed more than a thousand men with early-stage prostate cancer for several years and found men who ate even less than a single egg a day “appeared to have twice the risk of prostate cancer progression, such as metastasizing into the bones.” They found that poultry eaters fared even worse. “Men with more aggressive cancer who regularly ate chicken and turkey had up to four times the prostate cancer progression risk.”
- Eat cruciferous vegetables such as broccoli, brussels sprouts, cabbage, cauliflower, or kale. The Harvard study cited above also found that “less than a single daily serving of [cruciferous vegetables] may cut the risk of cancer progression by more than half.”
- Eat more fiber (which you will if you eat more fruits, vegetables, whole grains and legumes).
The World Cancer Research Fund and the American Institute for Cancer Research, compiled the most comprehensive summary of evidence on diet and cancer ever, which recommends we “eat mostly foods of plant origin to help prevent cancer. This means centering one’s diet around plant foods. Not just whole grains and beans every day, but every meal.”2
Considering that no more than 2 percent of all human cancer is attributable to purely genetic factors, in addition to getting screened where it makes sense, this is good advice for everyone.
References
- Anti-Aromatase Activity of Phytochemicals in White Button Mushrooms (Agaricus bisporus). Shiuan Chen, Sei-Ryang Oh, Sheryl Phung, Gene Hur, Jing Jing Ye, Sum Ling Kwok, Gayle E. Shrode, Martha Belury, Lynn S. Adams and Dudley Williams.
- World Cancer Research Fund, American Institute for Cancer Research. Food, nutrition, physical activity, and the prevention of cancer: A global perspective. Chapter 12: Public health goals and personal recommendations.
WholeBlue Living's Defining Facts - January 2018
Coconut oil: the good, the bad, and the ugly
Quick, name an oil that’s good for you.
If you said coconut oil, you may be right. Or wrong. It depends on what you are using it for and what research you’re looking at.
Search coconut oil on the internet and you will discover claims that it can cure or treat nearly everything, including: diabetes, heart disease, chronic fatigue, Crohn’s disease, irritable bowel syndrome (IBS), Alzheimer’s disease, Parkinson’s disease, dementia, thyroid conditions, energy problems and immune system issues. Some people even claim it helps them to lose weight or lower cholesterol.
But tucked among those bold claims in your search results, you’d also find statements like this one from the American Heart Association in a 2017 USA Today article: “Because coconut oil increases LDL cholesterol, a cause of CVD [cardiovascular disease], and has no known offsetting favorable effects, we advise against the use of coconut oil.”1
And if you search that article, you will find numerous sources that “debunk” that news, like this one, that says, “Why we should not trust the American Heart Association.”
So what should you believe?
The answer lies in your cholesterol level. The healthier your cholesterol levels, the lower your risk of heart disease. In fact, in the landmark Framingham Heart Study, William Castelli, M.D., the cardiologist who established the study, noted that “no one in the study…with a cholesterol level of under 150 has suffered a heart attack.”2
While the level of 150 is currently disputed as “heart attack proof” lower cholesterol levels appear to not help our hearts, but may also minimize risk of related conditions such as stroke and dementia (like Alzheimer’s disease). According to Dean Sherzai, MD, PhD, a medical pioneer who treats Alzheimer’s disease with lifestyle medicine, “Ninety percent of us can avoid getting Alzheimer’s.”3
Since achieving a low cholesterol level usually requires a whole-food, plant-based diet, the risk of non-cardiac-related diseases will likely fall as well. Those with super-low cholesterol levels tend to live fully to the end instead of languishing for months or years in nursing homes or hospitals before finally succumbing to death.
The American Heart Association recommends eating “no more than 6% of saturated fat as part of total daily calories for those who need lower cholesterol.” That’s about 120 calories for someone who should consume about 2,000 calories a day to maintain their weight, or about 11 to 13 grams of saturated fat.1
Saturated fat primarily comes from animal products, which also contain dietary cholesterol. Plant foods that contain saturated fat include coconut, coconut oil, palm oil and cocoa butter.
So the question is not whether one should eat coconut oil but whether a person can maintain a Standard American Diet (SAD) and keep daily intakes of saturated fat under 11 grams, and cholesterol under 150. That answer is likely no, considering the following sources of saturated fat from the SAD:
• Plain, low-fat yogurt (8 oz), 2.27 grams
• Plain, whole-milk yogurt (8 oz), 4.76 grams
• One egg, 1.55 grams
• One teaspoon butter, 2.43 grams
• One teaspoon coconut oil, 4 grams
• One grilled (no oil), boneless, skinless chicken breast .841 grams
• Sharp cheddar cheese (1 oz) 5 grams
• 1/4 cup coconut milk, 10 grams
• Boneless lamb (3 oz) 7.47 grams
• One slice bacon, 1 gram
• Burger King bacon and cheddar BK toppers 11 grams
• One Krispy Kreme original glazed doughnut, 5 grams
• One Pepperidge Farm soft-baked sugar cookie, 2.5 grams
• McDonald’s Southwestern Salad, 3 grams
Other oils aren’t much better. A study published in Nutrition, Metabolism and Cardiovascular Diseases in 2007 found that all oils have a damaging effect on endothelial function after each meal, independent of what type of oil, or whether the oil was fresh, or deep fried. The endothelial is the lining of the heart and blood vessels. Loss of proper endothelial function can lead to cardiovascular disease. The oils studied included olive, soybean and palm.4
Another study found that extra virgin olive oil keeps a fraction of its anti-inflammatory phytonutrients found in the olive fruit, and therefore doesn’t appear to induce inflammation, but that was compared to butter.5
Other studies show conflicting results between extra virgin olive oil and regular olive oil, primarily due to study design. The better-designed studies tend to show benefit to olive oil. However, these studies looked at olive oil in the context of the Mediterranean diet.
It is unknown whether the olive oil provided benefit to the heart or if that was due to the number of whole grains, fruits, vegetables, beans and walnuts included in the study diet. Numerous other studies indicate that diets rich in these foods provide some protection against direct impairment of endothelial function produced by high-fat foods, including olive oil. It may be that the health improvements were in spite of the oil, not because of it.6/
But back to coconut oil. Some claim that coconut oil can help with weight reduction. One study that looked at that issue found it no better than other oils. Unfortunately, the coconut oil group did have a significant increase in insulin resistance, which is what eventually causes type 2 diabetes. This happened even though the study participants were told to increase fruits and vegetables, and cut down on sugars and animal fat. The participants also walked 50 minutes a day, four days a week.7
Coconut oil proponents often rely on studies that show that Pacific islanders who eat more traditional coconut-based diets are slimmer than those who eat diets without as much coconut. But, a closer look at the study reveals that the comparison is between those who have “a high intake of local foods, including…coconut products, and [a root vegetable like] taro, and low intake of processed foods, including potato chips and soda.”8
The bottom line is if your eating habits are so healthy that your total cholesterol is under 150 or your LDL cholesterol is under 60, coconut oil may not be a problem. Unlike saturated animal fats, it doesn’t cause a spike in inflammation immediately after consumption. But if you’re trying to improve your cholesterol, coconut oil may be another to avoid.
But don’t throw it away yet. Some sources claim that external uses of coconut oil are beneficial. For example, it may help to make your hair shiny, and improve dry skin. Other sources claim coconut oil can help to speed up wound healing.
References
- USA Today.
- Newsmax.com
- Bluezones.com
- Rueda-Clausen CF1, Silva FA, Lindarte MA, Villa-Roel C, Gomez E, Gutierrez R, Cure-Cure C, López-Jaramillo P. Olive, soybean and palm oils intake have a similar acute detrimental effect over the endothelial function in healthy young subjects. Nutr Metab Cardiovasc Dis. 2007 Jan;17(1):50-7. Epub 2006 Mar 20.
- Tentolouris N1, Arapostathi C, Perrea D, Kyriaki D, Revenas C, Katsilambros N. Differential effects of two isoenergetic meals rich in saturated or monounsaturated fat on endothelial function in subjects with type 2 diabetes. Diabetes Care. 2008 Dec;31(12):2276-8. Epub 2008 Oct 3.
- Buckland G1, Travier N, Barricarte A, Ardanaz E, Moreno-Iribas C, Sánchez MJ, Molina-Montes E, Chirlaque MD, Huerta JM, Navarro C, Redondo ML, Amiano P, Dorronsoro M, Larrañaga N, Gonzalez CA. Olive oil intake and CHD in the European Prospective Investigation into Cancer and Nutrition Spanish cohort. Br J Nutr. 2012 Dec 14;108(11):2075-82.
- Assunção ML1, Ferreira HS, dos Santos AF, Cabral CR Jr, Florêncio TM. Effects of dietary coconut oil on the biochemical and anthropometric profiles of women presenting abdominal obesity. Lipids. 2009 Jul;44(7):593-601. doi: 10.1007/s11745-009-3306-6. Epub 2009 May 13.
- DiBello JR1, McGarvey ST, Kraft P, Goldberg R, Campos H, Quested C, Laumoli TS, Baylin A. Dietary patterns are associated with metabolic syndrome in adult Samoans. J Nutr. 2009 Oct;139(10):1933-43. doi: 10.3945/jn.109.107888. Epub 2009 Aug 26.


Weight gain and food “addiction”
Certain substances in our brains can make us feel as though we are addicted to food, especially unhealthy food. When scientists first discovered these substances, they hoped to create a drug that could slim people. However, the more research they conducted the more they realized it’s not that simple.
Numerous factors affect weight gain, among them brain chemistry, exercise levels, sleep, genetics, daily movement and food choices. Except for a very tiny percentage of people who have rare genetic or other diseases that cause them to gain weight, everyone can get to their ideal weight, but not everyone will find it easy.
Let’s look at each of them.
Brain chemistry
Scientists have discovered a complex web of brain circuitry and chemicals that regulate and affect what we eat, how much we eat and whether we are overweight. Stephan J. Guyenet, PhD, does an excellent job explaining these in his book, The Hungry Brain.
One of the components Guyenet focuses on is called leptin, also known as “the hormone of energy expenditure.” Leptin helps to regulate energy balance by inhibiting hunger and is opposed by the actions of the hormone ghrelin, the “hunger hormone.” Together, the hormones act on different brain receptors to regulate appetite and achieve energy homeostasis.
Although regulation of fat stores is deemed to be the primary function of leptin, it also plays a role in other physiological processes. A problem with leptin or ghrelin levels can cause problems with over- or under-eating.
Exercise
The next factor is exercise. But it’s not as simple as many believe.
The scientific evidence has shown that exercise does cause fat loss, but John Blundell, professor of psychobiology at the University of Leeds, demonstrated that not everyone loses the same amount of fat when they exercise.
At the end of a 12-week study period, the average participant had lost more than eight pounds of fat . . . however, the range included a loss of 21 pounds by one participant, a gain of six pounds by another and only two pounds lost for two others.
“Those who lost less weight than expected were inadvertently increasing their calorie intake in response to exercise,” Blundell said. “Those who lost as much or more weight than expected actually decreased their calorie intake in response to exercise. About half ate more as a result of the exercise and about half ate less.”1
In other words, when trying to lose weight through exercise, people will need to also be careful it doesn’t make them want to eat more.
Sleep
Sleep also affects weight gain. In general, the less sleep a person gets, the more likely that person is to gain weight. A 2011 study conducted at the New York Obesity Research Center at Columbia University concluded that when sleep deprived, study volunteers ate nearly 300 calories more per day than when they were well rested.2
Genetics
We’ve all heard the “excuse” that some people can’t help being overweight because of genetics. In his book, Guyenet said, however, that even if we carry fat genes, we are not destined to be fat. They do, though, make us susceptible when we are surrounded by a fattening environment.
Daily movement
People who naturally move a lot during the day tend to be thinner. James Levine, an endocrinologist who works with the Mayo Clinic, and Arizona State University conducted a controlled “overfeeding” study. His team demonstrated the concept of “non-exercise activity thermogenesis (NEAT),” a form of calorie-burning also known as fidgeting. Levine said, “When certain people overeat, their brains boost calorie expenditure by making them fidget, change posture frequently, and make other small movements throughout the day.”3
Food choices
Researchers have found that what we eat is also an important factor in weight loss. Many people believe that a high-protein diet is necessary for weight loss. However, a 2005 study led by University of Washington researcher Scott Weigle demonstrated that while high-protein diets can lead to weight loss, it’s not because of a reduction in carbohydrates. Weigle’s team increased protein at the expense of fat, not carbohydrates. In fact, high-carbohydrate diets can also lead to weight loss.4
Researchers also found that a bland diet leads to less consumption, even when research subjects are allowed to eat as much as they wish. A weight-loss study Michel Cabanac led at Laval University in Canada found that those who were required to control their portions developed “the expected hunger response to weight loss” but those who were told they could eat what they wanted from bland choices didn’t. They “reduced their intake voluntarily and were always in good spirits.”5
For those who want to lose weight, the research suggests the best first step is to imagine yourself in the future, what you want to be like. (See blog post on change.) When people can pit their present self versus their future self, a technique called episodic future thinking, they have better success. For example, the next time you are tempted to eat a pastry, first imagine positive events in the future, such as running fast or keeping up with your grandchildren.
Several other factors to weight management are within a person’s control as well. These include the following six things:
1. environment
2. appetite
3. food rewards
4. sleep
5. moving
6. stress
Environment. If you want to change what you eat, you need to change what you are around. First, get rid of everything that tempts you at home. Outside your home the concept is easier said than done. After all, you can’t tear down that tempting fast-food restaurant you pass every day. But if you bring some heathy food along with you wherever you go, you’ll have less reason to stop.
Appetite. The science indicates you can manage your appetite by managing the foods you eat. For regular meals, choose foods that are as close to their most whole state as possible. For example, eat whole grains, not refined. Fruit, not juice, and olives not olive oil. Also, manage when you eat food. If you are always “starving” when you come home from work, prepare an afternoon snack that will slow down the hunger pangs. The research demonstrates that we make our worst food choices when we’re the most hungry.
Food rewards. Our brains value foods that are calorie-dense combinations of fat, sugar, starch, protein, salt and other less-than-healthy things. Beware, because the research demonstrates that the more of these unhealthy foods we eat, the more we want. Instead, make it your habit to fill up on whole-food, plant-based foods, and you will be less tempted by the other foods, especially if you follow the other tips.
Sleep. In the United States we often consider it a badge of honor if we can get by with just a few hours of sleep. But for the majority of us, such lack of sleep increases our weight and shortens our lives. If you want to be the most whole you can be, get around eight hours of sleep every night.
Moving. Moving your body does not need to mean structured exercise, but it can. Our ancestors farmed and walked and did household chores by hand. They didn’t need the gym. Walking with a friend, playing sports and taking the stairs instead of the elevator are all ways of moving that are easy.
Stress. Last but certainly not least, it is important to manage the daily stresses of life. There are numerous ways to do this including mindful relaxation techniques, exercise, nature, hanging out with friends and more. If you already do some of those things and you’re still stressed, you may need to look deeper and speak to a counselor.
So, imagine where you want to be in six months or a year or more, design an eating plan you can live with for the long haul and figure out the steps that will get you there. If you need help, sign up for the free Whole New You workshop, only available twice a year.
References
- N.A. King, M. Hopkins, P. Caudwell, R.J. Stubbs, and J.E. Blundell, “Individual variability following 12 weeks of supervised exercise: identification and chararcterization of compensation for exercise-induced weight loss.” International Journal of Obesity 32, no. 1 (January 2008): 177-84.
- M.P. St.-Onge, A. L. Roberts, J. Chen, et al. “Short sleep duration increases energy intakes but does not change energy expenditure in normal-weight individuals. Journal of Clinical Nutrition 94, no. 2 (August 2011): 410-16.
- J.A. Levine, N.L. Eberhardt, M. D. Jensen, “Role of nonexercise activity thermogenesis in resistance to fat gain in humans,” Science 283, no. 5399 (January 8, 1999): 212-14.
- D.S. Weigle, P.A. Breen, C.C. Matthys, H.S. Callahan, K.E. Meeuws, V.R. Burden, at al., “A high-protein diet induces sustained reductions in appetite, ad libitum caloric intake, and body weight despite compensatory changes in diurnal plasma leptin and ghrelin concentrations.” American Journal of Clinical Nutrition 82, no. 1 (July 2005):41-48.
- M.Cabanac, E.F.Rabe. “Influence of a monotonous food on body weight regulation in humans.” Physiology & Behavior Volume 17, Issue 4, October 1976, Pages 675-678.
WholeBlue Living's Defining Facts, December 2017
Should you eat a gluten-free diet?
Browse the aisles of any grocery store in the United States today and you will see hundreds, if not thousands of products aimed at specialty diets such as gluten-free. With the increasing demand for such products, some consider allergies or intolerances a growing public health concern.
According to the Statistics Portal, the market for gluten-free foods in particular is growing. The site notes that by 2020, the market is projected to be valued at $7.59 billion. Gluten-free food accounted for 6.5 percent of all U.S. food sales in 2015, up from 2.8 percent in 2013.1
Those who purchase gluten-free foods include people suffering from celiac disease or gluten sensitivity, or those who identify as very health conscious. Celiac disease, sometimes known as gluten intolerance, is a genetic disorder. Symptoms can include diarrhea, weight loss, and malnutrition or isolated nutrient deficiencies with no gastrointestinal symptoms. Those affected suffer damage to the villi in their intestines. Microscopic amounts of gluten can cause symptoms in those with the disease.2
In North America, about 8 percent of the population follows a wheat- or gluten-free diet, whether or not they have celiac. Around 64 percent of U.S. consumers consider such a diet “very healthy” or “somewhat healthy.”1
With such an increase in gluten-free products, one would assume the rates of diseases such as celiac are rising as well. A study published in the July 2012 issue of The American Journal of Gastroenterology evaluated celiac’s prevalence in the United States. The researchers found an increase between 1988 and 2012.
Still, the overall rate of Americans who truly have the disease is relatively small, around 1 percent of the population.
Is it all in your head?
If only 1 percent of Americans have celiac, why are more than 6 percent eating a gluten-free diet? Sheila Crowe, M.D., a spokesperson for the American Gastroenterological Association and a professor in the division of gastroenterology at the UC San Diego School of Medicine, addressed the question in an article on the Celiac Disease Foundation’s website.3
“There’s more of a modern concern that gluten is somehow not good for us,” she said, but added that there’s little evidence proving gluten-free means good health.
Some say humans don’t fully digest wheat, that it’s pro-inflammatory, and that it can cause “leaky gut syndrome,” but there is little evidence cited to back up those claims. In fact, the opposite may be true.
The real problem comes, according to the researchers, when people have celiac disease but are unaware of it—that’s around 1.4 million Americans. It can also be a problem for those who haven’t been diagnosed with celiac—about 1.6 million Americans—but who are on a gluten-free diet anyway. Both groups may suffer health consequences.
There are two other groups that should avoid wheat or gluten. The first is those who have a wheat allergy. The other includes people who suffer health problems similar to people with celiac, such as chronic diarrhea, but have no clinical evidence of the disease.
In 1980, researchers in England reported on just such a population. At the time, the medical profession was skeptical. Patients who claimed this type of non-celiac gluten sensitivity were commonly referred to psychiatrists because they were thought to have a mental illness (even though subsequent psychological testing found no evidence of that).4
But in 2011, a double-blind, randomized placebo-controlled trial found that some patients have irritable bowel symptoms when they eat gluten, despite not having celiac disease.5
When the issue was studied in a larger trial in Italy in 2012, researchers found that for some subjects, there was a significant benefit to staying on a wheat-free diet, which confirmed the existence of a non-celiac wheat sensitivity, not necessarily a gluten sensitivity. The reason researchers are finding it tough to tease out the real culprit is that people who are sensitive to wheat, such as those in the 2012 study, typically have a variety of food sensitivities, such as to cow’s milk protein or eggs.6,7
Risks of not being diagnosed properly
Getting the diagnosis right before choosing a gluten-free diet is important. People with untreated celiac could suffer from deficiency of several nutrients leading to problems like iron deficiency anemia, osteoporosis, fertility problems and nervous system problems.
Those with non-celiac sensitivity suffer from problems such as “foggy mind,” depression, ADHD-like behavior, abdominal pain, bloating, diarrhea, constipation, headaches, bone or joint pain, and chronic fatigue. Typically, their sensitivity is to wheat, or other foods, not gluten, but a diagnosis is important. In both cases, lack of a diagnosis often means needless suffering.
But avoiding gluten when you don’t need to may pose its own set of problems.
There is no scientific evidence to suggest that following a gluten-free diet has any significant benefits for those who are in the 99 percent. This means gluten and wheat protein is healthy for about 99 percent of the population, especially when those products are consumed in their most whole form.8
Instead, the evidence suggests that a gluten-free diet may adversely affect gut health in those without celiac disease, gluten sensitivity or wheat allergy, or cause other problems. For example, an article on LiveScience.com in May 2016 discussed the research specific to children, noting that, “There’s no scientific evidence that a gluten-free diet brings health benefits to people who don’t have celiac disease, wheat allergy or nonceliac gluten sensitivity.”9
For children, one of the harms comes from the added fats and sugars found in many gluten-free products. Some become obese or overweight after starting a gluten-free diet.
But the other harm from going gluten-free when it’s not medically warranted is mostly missed opportunity for a healthier life. Whole grains—including the gluten grains wheat, barley and rye—are linked to a reduced risk of coronary heart disease, cancer, diabetes, obesity and other chronic diseases. Eliminating them from your diet eliminates their benefits.8
The beneficial effects on our gut health include substances that act as prebiotics and feed our good bacteria, and the gluten itself, which may boost immune function. Gluten protein can also increase natural killer cell activity, which could be expected to improve our body’s ability to fight cancer and viral infections. In addition, high-gluten bread improves triglyceride levels better than regular gluten bread.10,11,12
Are you sensitive?
Today, a consensus panel of experts officially recognizes three gluten-related conditions: wheat allergy, celiac disease, and gluten sensitivity. How do you know if you are among the three?
First, if you have any of the symptoms of celiac or non-celiac, mentioned earlier, or if you have a relative with celiac, you should be tested for the disease. It’s a simple blood test. (The standard intestinal biopsy may not be necessary.)
But before you go, make sure you talk to your doctor first about eating gluten in the weeks before the test. Why? Because the first test for a formal evaluation of the disease is a blood test. People who eat gluten have higher than normal levels of certain antibodies in their blood. However, if you have been off gluten you would have lower levels for those antibodies.
If you do test positive, your doctor may also do other tests, or put you on a gluten-free diet, depending on your results.
If your test is negative for celiac, before going gluten free, first try a healthier diet by incorporating more fruits, vegetables, whole grains, legumes and beans while avoiding processed junk for at least three weeks. If a healthy diet doesn’t help, Michael Greger, M.D., next recommends ruling out other causes of chronic gastrointestinal distress such as an overgrowth of bacteria in the small intestine, fructose or lactose intolerance, or neuromuscular disorders like gastroparesis or pelvic floor dysfunction before going gluten-free.13
After all that has been tried, Greger then recommends trying a gluten-free diet, but sticking with it only if symptoms improve, and re-challenging with gluten from time to time.
No current data suggest that the general population should maintain a gluten-free lifestyle, but for those with a celiac disease, wheat allergy or sensitivity diagnosis, wheat- or gluten-free diets can be a life-saver.
References
- Statista.com
- Celiac.com
- Celiac Disease Foundation website.
- BT Cooper, GK Holmes, R Ferguson, RA Thompson, RN Allan, WT Cooke. Gluten-sensitive diarrhea without evidence of celiac disease. Gastroenterology. 1980 Nov;79(5 Pt 1):801-6.
- J R Biesiekierski, E D Newnham, P M Irving, J S Barrett, M Haines, J D Doecke, S J Shepherd, J G Muir, P R Gibson. Gluten causes gastrointestinal symptoms in subjects without celiac disease: A double-blind randomized placebo-controlled trial. Am. J. Gastroenterol. 2011 106(3):508 – 14 – quiz – 515.
- A Carroccio, P Mansueto, G Iacono, M Soresi, A D’Alcamo, F Cavataio, I Brusca, A M Florena, G Ambrosiano, A Seidita, G Pirrone, G B Rini. Non-celiac wheat sensitivity diagnosed by double-blind placebo-controlled challenge: Exploring a new clinical entity. Am. J. Gastroenterol. 2012 107(12):1898 – 906 – quiz – 1907.
- J R Biesiekierski, S L Peters, E D Newnham, O Rosella, J G Muir, P R Gibson. No effects of gluten in patients with self-reported non-celiac gluten sensitivity after dietary reduction of fermentable, poorly absorbed, short-chain carbohydrates. Gastroenterology 2013 145(2):320 – 8 – e1 – 3.
- J Slavin. Whole grains and human health. Nutr Res Rev 2004 17(1):99 – 110.
- Gluten-Free Diets May Be Risky for Kids
- G A Gaesser, S S Angadi. Gluten-free diet: Imprudent dietary advice for the general population? J Acad Nutr Diet 2012 112(9):1330 – 1333.
- G De Palma, I Nadal, M C Collado, Y Sanz. Effects of a gluten-free diet on gut microbiota and immune function in healthy adult human subjects. Br. J. Nutr. 2009 102(8):1154 – 1160.
- D J Jenkins, C W Kendall, V Vuksan, L S Augustin, C Mehling, T Parker, E Vidgen, B Lee, D Faulkner, H Sevler, R Josse, L A Leiter, P W Connelly, V Eulgoni. Effect of wheat bran on serum lipids: influence of particle size and wheat protein. J Am Coll Nutr. 1999 Apr;18(2):159-65.
- NutritionFacts.org
Daily health
Most people who switch to a whole-food, plant-based diet generally feel like they have more energy, and statistically they live longer.1,2
But will they ever get sick?
The short answer is yes. Switching to a plant-based diet is not a pass from common illness such as flu and colds. In an article on the subject published on the Center for Nutrition Studies website, Thomas Campbell, M.D., said, “It is difficult to find a compelling weight of evidence showing that any particular dietary pattern clearly prevents or reduces the severity of upper respiratory infections.”3
There is some evidence of a benefit from a plant-based diet in some circumstances, and lifestyle definitely plays a part, but it’s not all due to diet. Lifestyle factors such as heaviness matters in some cases. For example, those who are overweight may react to the flu shot.4 Other lifestyle factors such as daily gargling with green tea can make a difference, as can regular moderate exercise.5
However, what we eat is also very important. Eating certain foods, such as kiwis or nutritional yeast, can lower the rate or duration of upper respiratory infections.6,7
In fact, anyone who eats more of any kind of fruits and vegetables, whether they are vegetarians or not, appears to have a lower risk of getting an upper respiratory tract infection, like the common cold. Just one added apple a day may help keep you from needing to make a visit to the doctor.
The best approach to cold and flu season is the same for any other illness: Feed your whole self—body, soul and spirit—every day. For example:
- Regularly consume at least two cups of green leafy vegetables every day.
- Eat lots of non-leafy vegetables, legumes and fruits, as well.
- Avoid stress. Easy to think of, hard to do. But stress reduction techniques don’t have to be difficult or time consuming. De-stressors include spending time in nature (or just looking at pictures of it), spending happy time with people you love, exercise, doing an activity you love, or just playing with a pet.
- Avoid dairy foods, particularly if you or your child has chronic congestion, frequent sinus problems or recurring ear infections. If you want to know if this is a problem, eliminate all forms of dairy for one month and keep a diary of the results.
- Sleep. Don’t say, “I’ll sleep when I’m dead,” because you could end up becoming sick more often (and possibly dead more quickly). In a 2009 study, those who slept less than seven hours a night were three times as likely to get a cold as those with eight hours or more.5
References
- M J Orlich, P N Singh, J Sabate, K Jaceldo-Siegl, J Fan, S Knutsen, W L Beeson, G E Fraser. Vegetarian dietary patterns and mortality in Adventist Health Study 2. JAMA Intern Med. 2013 Jul 8;173(13):1230-8.
- T Huang, B Yang, J Zheng, G Li, M L Wahlgvist, D Li. Cardiovascular disease mortality and cancer incidence in vegetarians: a meta-analysis and systematic review. Ann Nutr Metab. 2012;60(4):233-40.
- Center for Nutrition Studies.
- Sheridan PA, Paich HA, Handy J, et al. Obesity is associated with impaired immune response to influenza vaccination in humans. Int J Obes (Lond) 2012;36:1072-7.
- T. Noda, T. Ojima, S. Hayasaka, C. Murata, A. Hagihara. Gargling for oral hygiene and the development of fever in childhood: A population study in Japan. J Epidemiol 2012 22(1):45 – 49.
- D C Hunter, M A Skinner, F M Wolber, C L Booth, J M Loh, M Wohlers, L M Stevenson, M C Kruger. Consumption of gold kiwifruit reduces severity and duration of selected upper respiratory tract infection symptoms and increases plasma vitamin C concentration in healthy older adults. Br J Nutr. 2012 Oct;108(7):1235-45.
- Meng F (2016) Baker’s Yeast Beta-Glucan Decreases Episodes of Common Childhood Illness in 1 to 4 Year Old Children During Cold Season in China. J Nutr Food Sci 6:518.
- Cohen S, Doyle WJ, Alper CM, Janicki-Deverts D, Turner RB. Sleep habits and susceptibility to the common cold. Arch Intern Med 2009;169:62-7.

November 2017 News from WholeBlue Eating
Give thanks with a grateful heart
With the U.S. holiday of Thanksgiving in November, we’re expected to be thankful during the month, or at least on the holiday itself. However, research indicates we would be best served to be thankful every day of the year.
An article in the Journal of Social and Clinical Psychology summarizes the gratitude literature, saying that gratitude may have the highest connection to mental health and happiness of any of the personality traits studied.
“Around 18.5 percent of individual differences in people’s happiness could be predicted by the amount of gratitude they feel,” researchers said.1
Another study found that “overall gratitude seems to directly foster social support, and to protect people from stress and depression, which has implications for clinical interventions.”2
A 2015 article on Psychology Today’s website, noted seven scientifically proven benefits to being thankful.3
- Thankfulness invites more relationships. According to a 2014 study published in Emotion, showing appreciation can help you make new friends. “The study found that thanking a new acquaintance makes them more likely to seek an ongoing relationship.”
- Thankfulness improves physical health. A 2012 study published in Personality and Individual Differences noted that “grateful people experience fewer aches and pains and report feeling healthier than other people.” In addition, they found that more-grateful individuals tend to exercise more often and are more likely to have regular check-ups.
- Thankfulness improves psychological health. Robert Emmons, a leading gratitude researcher, found that gratitude reduces numerous toxic emotions, including envy, resentment, frustration and regret. He says “gratitude heals, energizes, and transforms lives.”
- Thankfulness reduces aggression and enhances empathy. A 2012 study by the University of Kentucky found that even when others are not as kind, more grateful individuals are more likely to behave more kindly. Study participants experienced more sensitivity and empathy toward other people and a decreased desire to seek revenge, even when given negative feedback.
- Thankful people sleep better. According to a 2011 study published in Applied Psychology: Health and Well-Being, spending just 15 minutes writing a few grateful sentiments before bed, helped study participants sleep better and longer.
- Thankfulness improves self-esteem. A 2014 study published in the Journal of Applied Sport Psychology found that gratitude increased athletes’ self-esteem, leading to optimal performance. Other studies have shown that gratitude reduces social comparisons.
- Thankfulness increases mental strength. Research indicates that thankfulness may play a major role in overcoming trauma. For example, a 2006 study published in Behavior Research and Therapy found that Vietnam War veterans with higher levels of gratitude experienced lower rates of post-traumatic stress disorder. In another study, published in the Journal of Personality and Social Psychology in 2003, researchers found that gratitude was a major contributor to resilience following the terrorist attacks on Sept. 11, 2001.
Emmons also notes that “religions and philosophies have long embraced gratitude as an indispensable manifestation of virtue, and an integral component of health, wholeness, and well-being.”
His team is studying the spiritual connection further. Other research has found that “those who regularly attend religious services and engage in religious activities such as prayer . . . are more likely to be grateful.”4
So, this Thanksgiving, be thankful and be blessed. And if you want to continue the blessings for the rest of the year, make Thanksgiving 2017 the first day of a year of daily gratitude.
References
- Robert A. Emmons and Cheryl A. Crumpler (2000). Gratitude as a Human Strength: Appraising the Evidence. Journal of Social and Clinical Psychology: Vol. 19, No. 1, pp. 56-69.
- The role of gratitude in the development of social support, stress, and depression: two longitudinal studies. Wood, Alex M.; Maltby, John; Gillett, Raphael; Linley, P. Alex; and Joseph, Stephen. (2008) Journal of Research in Personality, Volume 42 (No. 4). pp. 854-871. ISSN 0092-6566.
- Psychology Today.
- Emmons, R.A. (2009). The John Templeton Foundation. In S.J. Lopez & A. Beauchamp (Eds.), Encyclopedia of Positive Psychology (pp. 988-990). New York: Oxford University Press.


Friends (and even relatives) may lead to longer lives
Your holiday parties may help you live a longer life. Or any other social or family gatherings, any time of the year.
We’ve known that for decades. For example, a 1969 study published in The Gerontologist concluded that “maintaining health, mental abilities, and satisfying social roles are the most important factors related to longevity.”1
The Gerontologist research was not unique. More recently, Blue Zone research has found similar results. Coined in the November 2005 National Geographic magazine cover story, Blue Zone refers to five geographic areas where people live statistically the longest. The areas include: Okinawa (Japan); Sardinia (Italy); Nicoya (Costa Rica); Icaria (Greece) and Loma Linda, California, specifically among the Seventh-Day Adventists.2
One characteristic the Blue Zone people shared is that people of all ages in the regions are socially active and integrated into their communities. In fact, communities in the United States that have sought to mimic the Blue Zone communities have seen “double digit drops in obesity, smoking, and body mass index; millions of dollars of savings in healthcare costs; and measurable drops in employee absenteeism.”
Susan Pinker, author of The Village Effect: How Face-to-Face Contact Can Make Us Healthier, Happier, and Smarter, relays similar research. She says the high number of centenarians in Sardinia (six times as many centenarians as the mainland and 10 times as many as North America) are not simply due to “a sunny disposition or a low-fat, gluten-free diet” but “their emphasis on close personal relationships and face-to-face interactions,” although diet plays a role.3
Pinker cites numerous research studies in her book, The Village Effect, that attribute more than just longevity benefits to developing and maintaining lasting relationships. Such interactions help in many ways, including: as a buffer to stress and illnesses like cancer and heart disease; a bolster to immune systems; stronger mental health; and more.
Independent of our social interactions, our religious practices also play a role. In a 2011 study published in Religion, Brain and Behavior, researchers noted that “people who practice a religion are happier, healthier, and live longer than atheists.”4
And the benefits start young. For example, a study first published in 2006 found that regular connection at meal time can even support literacy development. This and other studies on the topic “consistently show that family meals are a handy predictor of a kid’s vocabulary, reading scores, and academic achievement and whether or not he or she will get derailed by sex, drugs, binging and purging, depression or suicidal thoughts.”5
During this holiday season, accept those invitations to celebrate, whether a Thanksgiving meal, an evening meal, or just a night out with friends. Your life may depend on it.
References
- Gerontologist. 1969 Summer;9(2):103-8.
- The Blue Zones.
- The Guardian.
- Michael Inzlicht, Alexa Tullett, Marie Good “The Need to Believe: A Neuroscience Account of Religion as a Motivated Process” Religion, Brain and Behavior 1, No. 3 (2011).
- Catherine E. Snow, Diane E. Beals. New Directions for Child and Adolescent Development. First published: 13 March 2006.
October 2017 News from WholeBlue Eating
Are you veganish?
The number of people who are choosing to eat plants over animals is rising. Not as much in the United States as in the United Kingdom, but it’s going up nevertheless, especially among younger generations. According to The Guardian, the number of vegans in the UK has risen by 350 percent in the past decade. In 2006, 150,000 people in that country opted for a plant-based diet. Today, 542,000 do. The growth is due in large part to people who are 15 to 34 years old (about 42 percent of the total) compared to only 14 percent who are 65 years or older.1
In 2009 in the United States, only 1 percent of the population reported eating vegetarian or vegan. By 2014, 5 percent of the United States population claimed to eat a vegetarian diet.2
While those numbers don’t seem high, they don’t tell the whole story. In some cases people don’t claim to be vegan, and yet eat a diet filled mostly with plants. In addition, for a nation seemingly obsessed with statistics, data on vegetarianism is almost completely lacking.
What is a vegan? Or for that matter, what is “veganish” or vegetarian or whole-food, plant-based? Let’s start with the strange term and a little history and work from there. The term veganish was popularized by Kathy Freston through her book, The Book of Veganish. Co-authored with Rachel Cohn, the book is aimed at teens and college students, and is full of information about how to eat a plant-based diet, why you would like to, and recipes to teach you how.
Freston says that her term veganish allows for more flexibility because telling someone you are vegan can make them “feel defensive.” She goes on to describe a diet and lifestyle that has been historically known as vegan, with the caveat that we all have choice to not have to stick to it 100 percent.
According to “A Brief History of Veganism” published in Time magazine in 2008, “Veganism is an extreme form of vegetarianism,” with the term coined in 1944. The article goes on to tell how the “concept of flesh-avoidance can be traced back to ancient Indian and eastern Mediterranean societies.”3
In 1948 Catherine Nimmo and Rubin Abramowitz founded the first vegan society in the United States. In 1960, H. Jay Dinshah founded the American Vegan Society (AVS). But veganism can be traced back to the Biblical era. The book of Daniel, which many believe was written around 530 BCE, describes how Daniel and a few of his contemporaries chose to live only on a diet of food grown by seed.
A vegan does not eat any part of an animal or use anything that comes from an animal—so eggs, dairy and often honey are excluded, as are leather, fur or any other animal-derived consumables. By comparison, vegetarians do not eat chicken, pig, cow, fish, turkey or any other type of animal, but often include dairy and eggs in their diet.
While there are many similarities between a whole-food, plant-based diet and a vegan diet, there are some important differences. I have a story about a friend that illustrates at least one of these differences.
When a vegan-eating friend was in the hospital giving birth to her youngest child, she selected the vegan diet from the hospital’s option. For dinner she was intrigued by the offer of a vegan dessert, so she checked that menu item. She couldn’t wait to see what it was.
When the meal arrived she looked at her dessert first—two Oreo cookies. The cookies are vegan by the definition of the word, but definitely not plant-based.
A whole-food plant-based diet on the other hand, is not an ethical choice per se, but a choice to select the healthiest possible food options overall. The whole-food, plant-based eater may avoid all eggs, dairy, meat, and fish like a vegan but may also occasionally include small amounts of these foods, more like the “veganish” person.
A whole-food, plant-based diet focuses on fruits, vegetables, legumes, grains, nuts and seeds, in as whole a form as possible. In many ways a plant-based meal would qualify as vegan but those who follow such a diet are not necessarily vegan. For example, whole-food, plant-based eaters may still wear leather and have no moral issue with hunting or killing animals for food.
Which is the better option?
When people hear that someone is vegan or vegetarian, they often think those individuals are eating a more healthy diet. But the truth is, just as you can eat an unhealthy diet based on animal products, you can eat a very unhealthy vegan or vegetarian diet.
The new term, “whole-food, plant-based” implies health. Its emphasis is on whole foods, that is, unprocessed foods in their most whole forms. Those who eat this way avoid oils because they are processed, not whole. The term “whole-food, plant-based” is more a description of healthy eating than a label.
For example, a vegetarian meal could include donuts and high-sugar, high-fat yogurt for breakfast, a grilled cheese sandwich for lunch with nacho cheese Doritos, a candy bar for a snack, and pizza with diet soda for dinner. In fact, many of our college students eat like this. The vegan version might be a power bar for breakfast, french fries and a plant-based burger for lunch, a bag of potato chips for a snack, and deep-fried tofu, salad and nondairy ice “cream” for dinner.
In this example the vegan’s food is more health promoting than the vegetarian’s; however, it still includes quite a bit of processed or high-fat food. But when someone says they eat a whole-food, plant-based diet, they are in it for the health.
And don’t be confused by those who say they are “plant based.” For some that is the same as saying they are vegan. Ask what they consider to be plant-based, because if they are eating the type of diet described earlier they may be missing the point of the whole-food, plant-based lifestyle.
So even if your diet contains a small amount of animal foods, if the majority of your calories (90 percent or more) come from whole plant foods, it is likely a better option than a traditional vegetarian or vegan diet. Here’s how you can tell if a food is a whole food.
- Whole foods nourish
A whole food meal doesn’t make you feel sick when you’re done (unless you’re allergic to something in it). After a whole-food, plant-based meal, you feel satisfied, not stuffed.
- Whole foods are health-promoting
Animal proteins have been linked to diabetes and high blood pressure and a host of other illness. Processed foods like processed meats have been linked to cancer. Sugar can raise your blood triglyceride levels (a part of your cholesterol that should be low). It may be vegan, but it doesn’t do your body good.
- Whole foods are better for the environment
I never used to think much about the environment. I grew up surrounded by dairy cows. I believed milk does a body good. And you can produce a lot of milk per acre of land. While there is no hard and fast rule, about 20 acres of land is needed each year to grow the food for every 50 cows. With those same 20 acres, you can grow about 90 percent of the food needed to nourish about 1,500 people. On the other hand, those 50 cows could provide three glasses of milk per day for more than 2,000 people. (The average cow in the United States produces about 21,000 pounds of milk per year, or the equivalent of about 128 glasses of milk per day.) But we need more than milk. And vegetables do a lot more good for the body than milk. And growing alfalfa means a lot of water. A report from the Pacific Institute, a nonprofit research organization, noted that, “In 2010, the single largest user of water [in California] was alfalfa [feed for cattle], with an estimated 5.2 million acre feet of applied water. A large and growing amount of water was also applied to almonds and pistachios, which together used 3.8 million acre feet of water.”
There are other ways the whole foods are better for the environment. Cows produce waste material that can be damaging to the environment. Plants produce vegetation. Whatever can’t be eaten can be recycled into the earth via composting. Plants produce carbon dioxide, a colorless and odorless gas that is vital to life on Earth. Cows produce methane, which is not toxic when inhaled (regardless of how bad it smells), but it can produce suffocation by reducing the concentration of oxygen inhaled.
So the question remains, are you veganish?
References


Depressing research on depression
and some exciting research, too
The leading cause of disability in the U.S. for ages 15 to 44 is major depressive disorder. In any given year, about 6.7% of the U.S. adult population is afflicted with the disorder, with more women than men suffering from it. The World Health Organization notes that depression is the most common illness worldwide and the leading cause of disability. An estimated 350 million people globally are affected by it.1
Major depressive disorder, also known as clinical depression, can cause severe symptoms that affect how you feel, think and handle daily activities, such as sleeping, eating, or working. It’s not just feeling sad or normal grief. In addition, the disorder has different forms. The most common are:
- Persistent depressive disorder (also known as dysthymia). This form lasts at least two years and may cycle with episodes of major depression along with periods of less severe symptoms.
- Perinatal depression. This form occurs during or after giving birth. Unlike the “baby blues,” with the more serious perinatal depression, the feelings of extreme sadness, anxiety and exhaustion make it difficult for the new mothers to care for themselves or others.
- Psychotic depression. This form occurs when a person has severe depression plus some form of psychosis, the symptoms of which often have a depressive “theme.”
- Seasonal affective disorder (SAD). This form generally occurs during the winter months when there is less natural sunlight, and lifts during spring and summer.
To be diagnosed with any of these, a person must experience some of the following signs and symptoms most of the day, nearly every day, for at least two weeks:
- Persistent sad, anxious, or “empty” mood
- Feelings of hopelessness, or pessimism
- Feelings of guilt, worthlessness, or helplessness
- Loss of interest or pleasure in hobbies and activities
- Decreased energy or fatigue
- Difficulty concentrating, remembering, or making decisions
- Thoughts of death or suicide, or suicide attempts
- (For more symptoms, please visit: the NIMH)
There is a lot of variability in what symptoms people with depression experience. If you think you may be suffering from it, consult with a health professional. Some medical conditions such as thyroid problems, a brain tumor or a vitamin deficiency can mimic symptoms of depression, so it is important to rule out general medical causes.2,3
Treating depression
Clearly, depression can be debilitating. However, it is treatable, often with good results, especially when caught early. The approach to treating depression is consistent across major health organizations such as the American Psychiatric Association and the National Institutes of Health. They note that treatments include: drugs, electroconvulsive therapy and psychotherapy.4
There are more effective treatments than these three commonly listed ones. The health organizations give some of them a nod by including them in their “self help” section, but given they are all backed by sound research, perhaps they should be moved to the front of the treatment line. These options fall under three primary categories: diet, exercise and energy psychology.
Diet
A study published in the American Journal of Health Promotion demonstrated how a plant-based diet can improve not only depression, but anxiety, fatigue and more. The 18-week study analyzed the health benefits of adopting a plant-based vegan diet in a corporate setting, specifically GEICO employees.5
The 292 participants were either overweight or struggling with type 2 diabetes. Participants of the study who ate the plant-based diet alleviated symptoms of anxiety, depression and fatigue, and improved their productivity at work and outside of work. The researchers concluded that “a dietary intervention improves depression, anxiety, and productivity in a multicenter, corporate setting.”
The benefits didn’t stop at improved mood. Over the course of the 18 weeks, the employees lost an average of 10 pounds, lowered LDL cholesterol levels by 13 points, and those with diabetes saw improved blood sugar control.
Other research has found that “frequent consumption of vegetables appears to cut one’s odds of depression by more than half.” And in this study, frequent was defined as merely eating vegetables three or more times a week.6
But eating vegetables even more than a few times a week and lowering animal protein may have even better results. A 2012 study published in Nutrition Journal, found that eliminating animal products, not just adding more vegetables, improved mood within two weeks.7
Improved depression for people on plant-based diets could also be from what’s in the plants—a class of phytonutrients that literally can get in our heads by crossing the blood-brain barrier. A review in the journal Nutritional Neuroscience suggests that eating lots of fruits and vegetables may present “a noninvasive, natural, and inexpensive therapeutic means to support a healthy brain.”8
This effect was seen in a study of nearly 300,000 Canadians, published in Preventive Medicine, that found that “greater fruit and vegetable intake was significantly associated with lower odds of depression.” The researchers concluded that because the high intake of fruits and vegetables is rich in antioxidants, it may dampen the detrimental effects of oxidative stress on mental health.9
Exercise
Aerobic exercise is another non-drug form of treatment for depression. Some studies found it comparable to antidepressant medication. For example, a study published in 1999 in the Archives of Internal Medicine looked at men and women over age 50 who suffered from major depression. They were randomly assigned to either an aerobic exercise program for four months, or a group that took the antidepressant drug called Zoloft.
Within four months, the drug group came down to normal on the depression scale they used. Which is what is expected from the antidepression drugs. The exercise-only group on the other hand, had the same powerful effect.10
A later study, published in 2007 in the Journal of Psychosomatic Medicine, also looked at antidepressant medication (in this case sertraline) compared to exercise, and added two other control groups: a placebo group and an unsupervised, “exercise at home” group. These researchers also found that exercise seems generally comparable with patients who receive medication for major depressive disorder, whether people exercised in a group or at home.11
Energy psychology
A third alternative option that has shown good results is energy psychology. In one study, the Emotional Freedom Technique, or EFT, was examined. In EFT work, clients tap or otherwise stimulate their acupuncture points to help clear trauma memory and emotion.
A study published in a 2005 issue of Counseling & Clinical Psychology Journal, looked at its usefulness in depression and found, “There was a statistically significant decrease in all measures of psychological distress as measured by the SA-45 from pre-workshop to post-workshop which held up at the 6 month follow-up.”12
Why the alternatives?
With three different options, some may wonder why organizations like the American Psychiatric Association still focus primarily on antidepressant medication, electroconvulsive therapy and psychotherapy. Especially since some depression medications have debilitating side effects, including death, that the other three options don’t have. Sometimes the medications themselves can lead to suicide in some patients.13
Perhaps even more concerning, results from the Nurses’ Health Study, published in 2009 in the Journal of the American College of Cardiology, examined whether there was a correlation between depressive symptoms, the use of antidepressant drugs and sudden cardiac death in 63,469 women who were free from any coronary disease, stroke or malignancy.
The researchers found that the more severe the depression the greater the risk of sudden heart failure. This was expected as research had demonstrated this finding in the past. However, these researchers found that the risk of death was not due to the depression alone, but to the medications used to treat it. Those women who were clinically depressed and taking antidepressant medications were more than twice as likely to experience sudden cardiac death compared to those women not taking the drugs.14
A report in the January 2013 issue of The British Medical Journal focused on a study conducted with more than 38,000 adult patients, all who had taken antidepressants or methadone and all who had electocardiograms recorded after taking these drugs. They also found cardiac problems related to some of the antidepressant medications.15
With the choice between antidepressant medications that can lead to heart problems and death, and options like exercise and diet, what will you seek first for yourself or a loved one, the next time the dark cloud of clinical depression strikes?
References
-
- Anxiety and Depression Association of America statistics.
- Psychiatry.org (American Psychiatric Association).
- National Institute of Mental Health website.
- Medical News Today.
- Am J Health Promot. 2015 Mar-Apr;29(4):245-54. doi: 10.4278/ajhp.130218-QUAN-72. Epub 2014 Feb 13.
- Public Health Nutr. 2012 Jun;15(6):1087-92. doi: 10.1017/S1368980011002977. Epub 2011 Dec 16.
- Nutr J. 2012 Feb 14;11:9. doi: 10.1186/1475-2891-11-9.
- Nutr Neurosci. 2012 May; 15(3): 127–133.
- Prev Med. 2013 Mar;56(3-4):225-30. doi: 10.1016/j.ypmed.2012.12.016. Epub 2013 Jan 4.
- Arch Intern Med. 1999 Oct 25;159(19):2349-56.
- Psychosom Med. 2007 Sep-Oct;69(7):587-96. Epub 2007 Sep 10.
- The Effects of EFT on Long-term Psychological Symptoms. Available at EBSCOHost.
- The Telegraph.
- Journal of the American College of Cardiology. Volume 53, Issue 11, March 2009 DOI: 10.1016/j.jacc.2008.10.060. Depression and Risk of Sudden Cardiac Death and Coronary Heart Disease in Women. Results From the Nurses’ Health Study.
- BMJ 2013; 346 (Published 29 January 2013)
September 2017 News from WholeBlue Eating
The problem with arsenic
How have you been celebrating National Rice Month this September? Eating rice crackers with nut butter? Trying a new variety of rice, like red or black or brown? Cooking with brown rice syrup? Or focusing on Whole Grain Month instead, which is also celebrated this month?
If you’ve been paying attention to nutrition research news lately, and you aren’t trying to avoid gluten, then you may be turning away from rice. Because it turns out there is a high amount of arsenic in most rice.
A tiny amount of arsenic — as small as a hundred milligrams — can kill you in an hour. That’s like the weight of a 10th of a feather. But there’s also arsenic exposure over time, called chronic arsenic poisoning. Chronic exposure, day after day for years at a time, can lead to a host of problems, one of the worst of which is cancer. Typical symptoms include diarrhea, headache, insomnia, loss of appetite and abnormal taste.
Arsenic is classified as a class I carcinogen, alongside things like cigarette smoke, formaldehyde, plutonium and asbestos. Long-term exposure to low to moderate arsenic levels has also been associated with heart attacks and strokes, as well as diabetes. While it’s not a proven cause and effect with those disease, it is a known carcinogen. It’s dangerous stuff.
Long-term exposure to arsenic can come through naturally contaminated groundwater, but higher levels are more likely to come through water or food contaminated through agriculture, or mining. And that’s how it got into our rice.
Rice accumulates 10 times more arsenic than other grains. That is why the arsenic levels in urine samples from those who eat rice are consistently higher than those who do not eat rice. Although, for the thousands of Americans who don’t eat rice at all, they’re still peeing out about eight micrograms of arsenic a day. It’s in the air; it’s in the water; there’s a little bit in nearly all foods. Add a cup or more of white rice a day, and exposure increases 65 percent.1
However, most Americans do not get most of their rice arsenic from eating just rice. They get it from eating things like crispy rice cereal. Organic brown rice syrup is another source, including that found in some toddler formulas. Rice milk is another source.
While all rice has arsenic, not all rice has high levels. For example, rice grown in California has 40 percent less arsenic than that grown in the south central United States. The difference is arsenic-based pesticides had been used on the cotton fields in that region for more than a century.
Today, arsenic pesticides are effectively banned, but millions of pounds of arsenic have already been mixed into the soil. It’s hard to eliminate it from the rice even if it’s grown organically. Rice fields are still so contaminated that producers have had to develop an arsenic-resistant strain. While the arsenic does not harm that strain, it is still absorbed into the plant and then into our bodies.2
Another top food source of arsenic has been chicken. Until 2013, producers fed arsenic-containing drugs to chickens. The arsenic then grew out into their feathers (which were then fed back to them as a slaughterhouse byproduct), their tissues, and then into our bodies. This explains why national studies found that those who eat more poultry have tended to have more arsenic flowing through their bodies.
The arsenic from the drugs in the feed can also get into our crops, into the air, and into the groundwater, then find its way into our bodies, whether we eat meat or not. And things grown with the help of chicken manure, like mushrooms, also contain high levels of arsenic. While these levels are starting to decrease as the implications of the ban take effect, levels are still high.
About a half million pounds’ worth of pure arsenic was dumped into the environment every year for many, many years — much of it onto our crops. It will take a long time for it all to dissipate.2
Arsenic is also an issue with some American wines. Even though arsenic use has been banned now, it still leaches from the soil, leading to “the pervasive presence of arsenic in wine [posing] a potential health risk.”3
There are no U.S. standards for arsenic in rice (or wine),4 but there are limits on things like municipal tap water and apple juice. And rice exceeds those limits. A generation could pass as we wait for the government to set standards; meanwhile, many recommend limiting rice consumption. In a 2012 report, Consumer Reports suggested no more than two servings of rice a week. Others recommend less.
The good news is, there are many other grains, some of which are also gluten free. The list includes: amaranth, barley, buckwheat, bulgur, corn, farro, freekeh, kamut, millet, oats, quinoa, rye, sorghum, spelt, teff, triticale and wild rice.
The Whole Grains Council suggests a number of ways to add more of these whole grains to your diet. The ideas include:
- Switch half the white flour to whole wheat flour in your regular recipes, or add up to 20 percent of another whole grain flour such as sorghum.
- Add half a cup of cooked wheat or rye berries, wild rice, brown rice, sorghum or barley to your favorite soup.
- Use whole corn meal for corn cakes, corn breads and corn muffins.
- Make risottos, pilafs and other rice-like dishes with whole grains such as barley, brown rice, bulgur, millet, quinoa or sorghum.
- Enjoy whole grain salads like tabbouleh.
- Look for cereals made with grains like Kamut®, kasha (buckwheat) or spelt.
In whatever form we eat them, whole grains are good for us. For example, just a single serving a day of oats or barley may lower our cholesterol, diabetes risk and more.5,6
So pick your (new) favorites and eat up.
References
- Epidemiology. 2015 Nov; 26(6): e65–e67.
- Yao L, Huang L, He Z, Zhou C, Lu W, Bai C. Delivery of roxarsone via chicken diet→chicken→chicken manure→soil→rice plant. Sci Total Environ. 2016 Oct 1;566-567:1152-8.
- Yang Z, Peng H, Lu X, Liu Q, Huang R, Hu B, Kachanoski G, Zuidhof MJ, Le XC. Arsenic Metabolites, Including N-Acetyl-4-hydroxy-m-arsanilic Acid, in Chicken Litter from a Roxarsone-Feeding Study Involving 1600 Chickens. Environ Sci Technol. 2016 Jul 5;50(13):6737-43.
- Wilson D. Arsenic Content in American Wine. J Environ Health. 2015 Oct;78(3):16-22.
- Am J Clin Nutr, October 2010 vol. 92 no. 4 733-740.
- Arch Intern Med. 2010 June 14; 170(11): 961–969.


Weighing in on childhood obesity
Several years ago, a reality television show featured an obese toddler. The toddler’s aunt called the show to help his mom, her sister, stop feeding him so much. He was 90 pounds at the time. (A child under 4 typically weighs less than 30 pounds.)
The camera showed the mother allowing her son an entire package of hot dogs plus other food for lunch. She said, “He’s hungry. I can’t deprive him.”
While that story was an extreme, it exemplifies the rising rates of childhood obesity in the United States. According to the CDC, obesity in youth is defined as a Body Mass Index (BMI) of greater than or equal to the age- and sex-specific 95th percentile of the CDC growth charts.
WebMD notes that obesity is “about much more than your clothing size or how you look. Your whole body feels it, from your joints to your heart, blood pressure, blood sugar, and other systems. The extra fat cells produce inflammation and various hormones, which boosts your odds of chronic medical conditions.”
Data from the National Health and Nutrition Examination Survey shows the upward trend for children.
- From 1963 to 1970, 4.2 percent of 6- to 11-year-olds and 4.6 percent of 12- to 19-year-olds were obese.
- In 1988, 11.3 percent of 6- to 11-year-olds and 10.5 percent of 12- to 19-year-olds were obese.
- In 2001, just over 16 percent of 6- to 11-year-olds were obese.
- In the last survey, from 2007 to 2008, 19.6 and 18.1 percent of 6- to 11- and 12- to 19-year-old kids were obese.
That’s bad enough, but it is just a measure of obesity. It does not include children who are merely overweight, which is defined as a BMI at or above the 85th percentile and below the 95th percentile for children and teens of the same age and sex.
The American Heart Association notes that “about one in three American kids and teens is overweight or obese” today. That’s a more than 100 percent increase since the early 1970s. By way of contrast, more than 36 percent of U.S. adults were considered obese during that same period.
For the children, the extra weight is causing physical and emotional health problems that previously weren’t seen until adulthood. Childhood obesity sets most people up for a lifetime of weight battles. According to a 2005 study in the journal Pediatrics, “Once an obese child reaches age 6, there is a greater than 50% probability that obesity will persist.”
But even if these overweight children slim down in adulthood, being overweight during the adolescent years predicts problems that include high blood pressure, type 2 diabetes, elevated blood cholesterol levels, low self-esteem, negative body image and depression. Excess weight during childhood has been linked to higher and earlier death rates in adulthood.1
Whether children are overweight or not, research has demonstrated that by the time we reach age 10, nearly everyone has fatty streaks in their arteries, which is the first stage of vascular disease such as heart disease or strokes. Plaques start forming in our 20s. When they get worse in our 30s, they can cause death from heart attacks, strokes and aneurisms, depending on where the plaques cause blockage.
Results from several studies, including a 2002 study in Minerva Pediatric, suggest that “prevention of coronary heart disease (CHD) should begin in adolescence or at least in young adulthood with control of the major established risk factors for adult CHD.”2, 3
One way to prevent heart disease is to begin with a “low-saturated-fat diet introduced in infancy and [maintain it] during the first decade of life.”4
But heart disease and thickening of our arteries are not the only problems that come from childhood obesity. Obese and overweight children are at risk for a number of other serious health problems, including Type 2 diabetes.
Type 2 diabetes was once called adult-onset diabetes, because it was rarely seen in childhood. But today rates are rising. According to research published in April 2017 in the New England Journal of Medicine, “The incidences of both type 1 and type 2 diabetes among youths increased significantly in the 2002–2012 period, particularly among youths of minority racial and ethnic groups.” Untreated, this can be a life-threatening condition.5
These younger diagnoses appear to be leading to more serious consequences. A 15-year follow-up of children diagnosed with Type 2 diabetes published in the World Journal of Diabetes in 2013 “found an alarming rate in young adults of blindness, amputation, kidney failure, and death in young adulthood.”6
According to the CDC, the causes of excess weight in youth are similar to those adults face. These include a combination of behavior, genetics and community. The CDC notes that “behaviors that influence excess weight gain include eating high-calorie, low-nutrient foods and beverages, not getting enough physical activity, sedentary activities such as watching television or other screen devices, medication use, and sleep routines.”
If you suspect your child is overweight, check out the CDC’s BMI calculator for child and teen and find out. Regardless of what you find, many organizations, such as Healthy Children (from the American Association of Pediatricians) have resources to help keep your child healthy.
And consider the recommendations of Dr. Benjamin Spock, perhaps the most influential pediatrician to date. In the last edition of his parenting book, Baby and Child Care, he advised a strict vegan diet for all children over the age of 2 years. He noted that they “can get plenty of protein and iron from vegetables, beans, and other plant foods that avoid the fat and cholesterol that are in animal products.”
For most of us, whether child or adult, the choice is not whether to live a stronger life in body, soul and spirit to prevent heart disease, prediabetes and other problems connected to weight. The choice is whether or not we want to reverse the conditions we already have. As Fatmanrants said in an Instagram post on September 22, 2017, “Change does not care about your past, color, race, religion, sex, financial, or social status. Change is a choice…everyone has the opportunity to choose.”
References
- T S Hannon, G Rao, S A Arslanian. Childhood obesity and type 2 diabetes mellitus. Pediatrics 2005 116(2):473 – 480.
- H. C. McGill Jr., E.E. Herderick. Atherosclerosis in youth. Minerva Pediatr 2002 54(5):437-447.
- C. A. McMahan, S. S. Gidding, G. T. Malcom, R. E. Tracy, J. P. Strong, H. C. McGill Jr. Pathobiological determinants of atherosclerosis in youth risk scores are associated with early and advanced atherosclerosis. Pediatrics 2006 118(4):1447 – 1455.
- O. T. Raitakari, T. Rönnemaa, M. J. Järvisalo, T. Kaitosaari, I. Volanen, K. Kallio, H. Lagström, E. Jokinen, H. Niinikoski, J. S. A. Viikari, O. Simell. Endothelial function in healthy 11-year-old children after dietary intervention with onset in infancy: The Special Turku Coronary Risk Factor Intervention Project for children (STRIP). Circulation 2005 112(24):3786 – 3794.
- N Engl J Med 2017; 376:1419-1429April 13, 2017
- T Reinehr. Type 2 diabetes mellitus in children and adolescents. World J Diabetes 2013 4(6):270 – 281.
August 2017 News from WholeBlue Eating
Don’t pass the salt!
I was born in a state where I learned at a young age to “salt first, taste later.” I have always liked my salt. So I was not happy to learn that there is a 17 percent increase in risk of cardiovascular disease for every gram of sodium one eats each day, even for people who have normal or low blood pressure.1
If you have high blood pressure (also known as hypertension) you have probably been counseled to cut down on the sodium. It is true, increased sodium intake is associated with increased blood pressure. And increased blood pressure leads to an increased risk of vascular diseases like strokes, aneurysms, and atherosclerosis.
But as the data show, too much sodium has also been tied to stomach cancer, kidney stones, bone loss, obesity, asthma, some autoimmune diseases like multiple sclerosis, as well as direct damage to our kidneys, arteries and hearts.
A Lancet article points out that “the most prominent dietary risks [are] diets low in fruits and high in sodium.” According to that article, 4.9 million deaths were attributable to diets low in fruit and 4 million to diets high in sodium.2
How much salt is too much?
The U.S. recommended daily value for sodium is less than 2,400 milligrams (mg) per day, equal to about a teaspoon of salt. The American Heart Association “recommends no more than 2,300 milligrams a day and an ideal limit of no more than 1,500 mg per day for most adults.” However, our bodies require about 460 mg.
Yet, most Americans over the age of 2 get much more than 2,400 mg a day. According to data published by the USDA,3 “the average sodium intake of the U.S. population aged 2 years and older was 3,330 mg per day,” with intake for 12- to 60-year-old males stretching as high as more than 4,000 mg per day.
A 1991 British Medical Journal article, indicated that a reduction of salt by about a half-teaspoon a day would “reduce the incidence of stroke by 22% and of ischaemic heart disease by 16%.” Of course, as mentioned earlier, numerous other health conditions would likely be helped as well.
How to reduce your salt intake
According to the FDA, “about 75% of dietary sodium comes from eating packaged and restaurant foods, whereas only a small portion (11%) comes from salt added to food when cooking or eating.” Therefore, one way to reduce sodium intake is to eat less packaged, processed and restaurant foods. But that is hard to do.
Let’s put this in context. A Southwest chicken salad at a famous fast-food restaurant has 1,070 mg. Its quarter-pound hamburger with cheese has a similar amount of sodium at 1,090 mg.
Eating “fast food” at home isn’t much better. Just a half-cup of vegetarian baked beans has 550 mg or more of sodium, and a pre-made vegan “burger” can have 280 mg or more. It doesn’t take a math whiz to see that one meal can give you up to half of your daily sodium intake.
How are you eating too much sodium?
According to a 2013 article in Nutrients,4 pizza is the top source of sodium for children and teens. For adults older than 51, it’s (store-bought) bread. For people ages 20 to 50, chicken contributes the greatest amount of sodium to their diet.
According to an article published in Cooking Light magazine, “a 4-ounce serving of what the industry calls ‘enhanced’ [raw] poultry can contain as much as 440 mg sodium. . . .500% more sodium than is found naturally in untreated chicken.”5 That’s before you season your cooking with salt.
While big industry pushes back on calls to reduce sodium in the foods they produce, there is something we can do at home. Those who want to significantly reduce their sodium must drop their consumption of meat and processed foods and couple that with eating a lot more vegetables, fruits, beans and whole grains.6
But for those of you who just want to eat a little less, with the hope for a larger dietary change in the future, there are some easy options. First, eat more unprocessed fruits, vegetables and whole grains. This means fresh fruit and vegetables instead of canned. Frozen is okay, but skip the pre-seasoned versions.
Not only do you fill your stomach (meaning less room for those processed foods) but the vegetables have other advantages, especially from leafy greens such as spinach, kale and chard. Eating these high-nitrate vegetables for a week could lower blood pressure by about four points. This can make a big difference. For example, just a 2 percent drop in blood pressure could prevent more than 10,000 fatal strokes each year.7
When you do buy processed foods, look for low-sodium items. According to NutritionFacts.org there are two tricks for figuring out whether the sodium level is low enough. The first is to look at the grams in the serving size compared to the milligrams of sodium. You want fewer milligrams of sodium than the serving size. For example, if the serving size is 100 grams, the food should contain less than 100 mg of sodium per serving.
The second option is to look for fewer milligrams of sodium than there are calories. For example, the vegetarian baked beans from the earlier example has 550 mg of sodium but only 130 calories. This is far too much.
And keep in mind, you really want less than this amount. That is, if all of your foods met the guidelines, you would still end up on the upper limit of sodium. So don’t pass the salt. Pass the spinach, please.
Note: If you are looking for some great ways to spice up your meal without salt, check out the Recipes section for this issue.
References
- Circulation. 2014 Mar 4;129(9):981-9.
- Lancet. 2012 Dec 15;380(9859):2224-60.
- USDA.gov
- Nutrients. 2013 May 28;5(6):1840-55.
- Cooking Light. 2011 Jan 14.
- J Am Diet Assoc. 2011 Jun;111(6):819-27.
- Nitric Oxide. 2013 Nov 30;35:123-30.


What’s for lunch?
This month and next, children are going back to school across the nation, and that means parents no longer have control over what goes in the mouths of their children at lunch time. Even toddlers will take healthy or unhealthy food from their neighbors (when children are older it’s called trading).
Nearly all schools across the United States offer some form of school lunch program, which usually includes the federally assisted meal program, called the National School Lunch Program. This program provides nutritionally balanced, low-cost or free lunches to children in public and nonprofit private schools and residential child care institutions. The program was established in 1946 under the National School Lunch Act.
Today’s National School Lunch program offers healthier choices, thanks to the Healthy, Hunger-Free Kids Act, implemented in 2016. The act was a key component of former first lady Michelle Obama’s, Let’s Move! initiative to raise a healthier generation.
Yet, healthy eating comes down to choice. A lunch menu for high school students in a Colorado school district this month offers a variety of options including a choice of: Asian bowl with rice and egg roll; hot wing basket; burrito or bowl; fruit and yogurt parfait; chicken tender basket; or flatbread sandwich or wrap, depending on the day of the week.
Students may also select from a hot sandwich such as a regular or spicy chicken filet, a hamburger or cheeseburger (presumably with an option for fries), a Mexican burger, or a ranch burger with onion rings.
Another choice is a signature baked pizza, with topping options of meatball, BBQ chicken, or veggie, Hawaiian, Mexican, Buffalo chicken, jalapeno, chicken, bacon, ranch, sausage, cheese, or pepperoni, depending on the day.
Students may also choose from the “Fresh Grab and Go” section that offers taco salad, Italian sub with chips, Buffalo chicken salad, turkey cheese sandwich, chicken Caesar salad, grilled cheese sandwich, chicken mandarin salad, American sub with chips, Italian deli salad, or ham and cheese sandwich, again, depending on the day.
So, what choice are students likely to make from that comprehensive line up? Pizza. According to a USDA report on the consumption of pizza, more than 25 percent of males and up to 20 percent of females aged 6 to 19 consumed pizza on any given day between 2007 and 2010. That report showed no difference between children of different races or ethnic groups.1
Once your children are at school, you can no longer make their food choices for them, but you can make it more likely they will choose something healthy. Instead of sending them to school with money to buy their own lunches, consider sending them with a healthy lunch you pack. It’s easier than you think, especially if you pack it the night before. [Note: This is a good idea for everyone who works outside the home.]
Following are some options. Remember, with a whole-food, plant-based diet, a snack is as healthy as a main course. Be creative in what you put together.
Main course ideas include:
- Nut-butter sandwiches on whole grain bread with banana, fruit-only jam, or lettuce
- Nut butter of your choice, spread on celery sticks with whole grain crackers on the side
- Avocado sandwich featuring avocado on whatever type of bread you like and other vegetables stuffed inside
- Whole-grain or multi-colored vegetable pasta with chopped vegetables
- Hummus with vegetables (such as cucumber, carrot, etc.) and whole-grain crackers for dipping
- Homemade burrito
- Black bean and rice salad on lettuce
- Mashed chickpea or edamame salad sandwich, or other kind of smashed-bean filling
- Any leftovers from food that was good the first time (e.g., homemade vegan pizza)
Consider using different breads such as tortillas or pitas with your sandwiches, or put the bread on the side. Just don’t assemble the sandwiches until morning so they won’t get too squishy.
Snack-type foods include:
- Beans, made simply and mashed or plain, depending what you or your child enjoys
- Low-sodium pretzels
- Dried fruit and/or seed or nut mix (depending on school policy).
- Homemade dry granola or other cereal
- Healthy snack bar
- Muffin or healthy breakfast-type cookie
- Homemade treats like bars or balls
For fruits and vegetables, use whatever is in season. Wash and cut it up so it will be easier to eat. Add a healthy, homemade oil-free dip for fruits or vegetables. People tend to eat more of the healthy fruits or vegetables if there is a dip.
If you arm your children with food from home they may still make trades, but in the process they’ll learn what healthy food is and what real choice looks like.
Reference
1.https://www.ars.usda.gov/ARSUserFiles/80400530/pdf/DBrief/11_consumption_of_pizza_0710.pdf
July 17, 2017 News from WholeBlue Eating
Relax!
We can do a lot of good for our bodies when we eat a whole-food, plant-based diet, but we are more than our bodies. We have a soul and a spirit, and they need to be fed well, too.
Just as hunger pains signal it’s time to eat food, when we begin to feel the effects of stress it’s time to nurture the emotional part of our souls. If we don’t, the wear-and-tear of stress will affect us in our bodies, souls and spirits.
Stress typically comes through emotions like worry, or fear, or grief, or abandonment, or resentment, or it can come through intellectual stressors like too much studying or problems with work. You can feel these kinds of stress through a headache, or tight muscles, or fatigue or even depression.
How you deal with stress is important to alleviating it. A whole-food, plant-based diet, along with exercise, will help the effects of stress on your body. There is much you can do to help eliminate your soul and spirit stress, too.
The most obvious is to remove the stressor, or remove yourself from the stressful situation. But in most cases this isn’t possible; stress is unavoidable. Instead we need to mitigate the stress. If we don’t, it can affect not only our physical health, but it can even change our genes.
Dr. Dean Ornish and his colleagues studied the integration of mind-body techniques such as yoga, meditation, stress management and group support. They found that “comprehensive lifestyle changes may ‘turn on’ the beneficial parts of the genome and ‘turn off’ the more harmful parts.”
Since such mind-body work can straighten out our genes, it implies that stress is able to get our genes off kilter in the first place. Thankfully, there are a number of things you can do to improve the health of your body, soul and spirit, like the things Dr. Ornish studied.
We can breathe deeply. Research shows that slow breathing a few minutes a day may have lasting beneficial effects on a number “of medical and emotional disorders, including asthma, irritable bowel syndrome, fibromyalgia and depression.”
For this technique, you take long, slow, deep breaths. As you breathe, you gently disengage your mind from distracting thoughts and sensations.
Music also reduces stress. Dr. Wendy Magee, an International Fellow in Music Therapy at the Institute of Neuropalliative Rehabilitation in London, described music as a “mega-vitamin for the brain.”
Researchers have found that music can bring lasting benefits to your state of mind, even after you’ve stopped listening. Breathing and heart rate can also be altered through music that activates the relaxation response.
In particular, religious chants like Gregorian chants, have shown beneficial effects. Monks at a monastery near Vienna, Austria, participated in a study looking at the effects of chanting. The monks’ heart rate and blood pressure dipped to the lowest point of the day when they were chanting. Previous studies demonstrated that chanting lowers blood pressure, increases performance hormone levels, and reduces anxiety and depression.
Nature is another source of both long- and short-term benefits. Nature can make you feel better emotionally and contribute to your physical well being. It can reduce your blood pressure, heart rate and muscle tension, and reduce the production of stress hormones. Scientists say it may even reduce mortality.
Research has shown that natural settings also reduce stress for victims of stroke, as well as for people who suffer PTSD and other anxiety disorders. Even short periods of time in nature can reduce symptoms of depression.
Other research has shown that being in nature, or even looking at pictures of nature scenes, can reduce anger, fear and stress, and increase pleasant feelings. Research done in hospitals, offices and schools has found that even one small plant in a room can have a significant impact on stress and anxiety.
Another great source of soul and spirit well being is healthy connection with other people. Such connections give us pleasure and influence our long-term health in ways every bit as powerful as a good diet.
Dozens of studies have shown that people who have satisfying relationships with family, friends and their community are happier, have fewer health problems and live longer. For example, married people are less likely to have a heart attack, according to the European Journal of Preventive Cardiology.
Other research demonstrated that long-term relationships mean better mental health for women and better physical health for men.
On the physical side, one study showed that married people have a three times higher survival rate post-heart surgery, compared with single people. Those who lack meaningful social ties, on the other hand, are more likely to be depressed and suffer later-life cognitive decline and increased mortality.
One study, which looked at data from more than 300,000 people, found that a lack of strong relationships increased the risk of premature death from all causes by 50 percent. That effect is roughly comparable to smoking up to 15 cigarettes a day, and it’s worse than being obese or physically inactive.
Breathing, nature, music and good friends and family can all help to reduce stress and make your body, soul and spirit stronger. So what can you do today to take advantage of these simple things? Commit to a daily nature walk? Listen to more music? Take five minutes to breathe?
The things to improve your soul health are simple, and they improve your body and spirit, as well.


I scream, you scream, are you addicted to ice cream?
On hot summer days, whenever I hear tinkly children’s music from around the corner, accompanied by the luring rumble of a small truck engine, I want to run for money. Even now that I don’t eat ice cream any more, and haven’t liked the ice cream truck’s offerings for years.
I’m probably not alone. Ice cream is very popular in the United States. In fact, President Ronald Regan designated July as National Ice Cream month in 1984.
About 90 percent of us consume around 6 gallons of ice cream every year, more than anyone in the world, with vanilla being the most popular flavor. About 9 percent of milk produced in the United States goes toward the production of ice cream. For reference, 12 pounds of milk are required to produce a single gallon of ice cream.
Why is ice cream so popular?
I used to think it was its combination of creamy smoothness and chill. Now I wonder if it’s only popular because of the “addiction” factor? The truth is, people who regularly eat ice cream—sugar and fat—have a deadened dopamine response in their brains, which is similar to when drug abusers have to use more and more of a drug to get the same high.
Even before looking at what the research says, we all know that ice cream is high in calories, which of course can lead to weight gain, which of course leads to health problems. One large vanilla shake at Baskin-Robbins has 1,420 calories and 48 grams of saturated fat, or more than double what’s in a Double Quarter Pounder at McDonald’s.
Light ice cream isn’t any healthier. It has at least 50 percent less fat than regular ice cream, but even light ice cream has too much fat.
The truth is, no ice cream is good for you. We know that. We say things like “I’m being decadent” or “Let’s indulge” when we eat it. For one, it’s one of the top contributors of cholesterol-raising saturated fat in your body.
In addition, milk—remember, a lot of milk goes into ice cream—is linked with an increased risk of Parkinson’s1, as much 17 percent for every cup of milk consumed daily. Milk consumption is associated with a significantly higher risk of hip fractures, cancer and premature death2,3.
Milk can even be blamed for acne4. Three Harvard studies linked dairy consumption with acne.
There are other options for creamy-cold summer refreshment. The difficult part is making the switch, especially letting go of the addiction.
Let’s look at one, a simple-to-make smoothie that tastes a lot like a strawberry shake. To make it, just combine a cup of cold soy milk, 3/4 of a cup of fresh strawberries, 1/4 cup of frozen strawberries and a ½ teaspoon of vanilla in a blender and blend until smooth. (In lieu of the frozen berries use 1 cup of fresh and add a few ice cubes.)
This drink will not only satisfy your cool craving (once you get over your addiction), it is so much healthier. Here are just three of those health benefits:
- In one study, the progression of esophageal cancer was reversed for 80 percent of patients who ate 1 or 2 ounces of freeze-dried strawberries every day for six months. (That’s equivalent to more than a pound of fresh.) So it’s a lot of strawberries, but these were patients who had active cancer.
- Strawberries also help to repair DNA damage, according to the results of at least one research study.
- Breast cancer survivors who eat soy foods have a significantly lower likelihood of cancer recurrence.
Let’s look at it another way. The following chart shows the nutrient content of the strawberry-soy “smoothie” compared to the nutrient content of a strawberry shake from a well-known fast-food restaurant. The fast-food milk shake contains cream and milk along with a bunch of ingredients you don’t need to put in your body. Oh, and some strawberries.
| Nutrient | 3-ingredient strawberry smoothie | Well-known strawberry shake |
| Calories | 120 | 510 |
| Cholesterol | 0 mg | 60 mg |
| Fat | 4 g | 15 g |
| Sodium | 85 mg | 170 mg |
| Protein | 8 g | 11 g |
| Vitamin A | 12% | 20% |
| Vitamin C | 100% | 2% |
| Iron | 6% | 0% |
| Calcium | 30% | 35% |
It’s easy to see what the better option is.
So the next time you are craving a cold creamy treat, go to the grocery store instead and stock up on your favorite berry flavors. It can be faster and less expensive to whip up something in your kitchen than going through the drive-through, and you’ll be smiling long after the last slurp.
References
-
Eur J Epidemiol. 2014 Sep;29(9):613-9. doi: 10.1007/s10654-014-9921-4. Epub 2014 Jun 4.
- BMJ. 2014 Oct 28;349:g6015. doi: 10.1136/bmj.g6015.
- NutritionFacts.org
-
Nestle Nutr Workshop Ser Pediatr Program. 2011;67:131-45. doi: 10.1159/000325580. Epub 2011 Feb 16.
June 20, 2017 News from WholeBlue Eating
Is Alzheimer’s disease preventable?
Alzheimer’s disease, indeed, any form of dementia, can be scary. It seems like it creeps up on a person. One day they’re fine, the next day memory loss.
Most people worry about losing their ability to think, reason and remember. Those who have witnessed a loved one suffer from dementia worry about this perhaps more than others. I know I have.
What makes the disease most chilling is there seems to be no way to avoid or treat it. Over two decades, more than 73,000 research articles published on the subject, yet little clinical progress made.
You’ll hear discussions connected to the disease, about plaques and tangles and exercise and losing weight and more, but very little about hope.
In 2015, approximately 29.8 million people worldwide suffered from Alzheimer’s disease. First described by, and later named after, German psychiatrist and pathologist Alois Alzheimer in 1906, the disease most often is diagnosed in people who are over 65 years old. Risk factors include genetic predisposition, depression and hypertension.1
According to Wikipedia, the cause is poorly understood. Until recently, I would have agreed. I always thought that dementia, including Alzheimer’s, was something you hoped you would never get, but would never know if you were at risk until you got it. Like a cold in the winter time, only much more insidious.
What changed my mind was the research on the connection between lifestyle factors, including diet, and Alzheimer’s disease and other forms of dementia. That research also shows that we have to prevent dementia early, before we can actually tell that someone has brain loss.
There seems to be a slow decline in brain function—and the buildup of those plaques and tangles—for decades before someone is diagnosed with Alzheimer’s.
Researchers conducted thousands of autopsies and saw what appears to be the first stages starting very early in life. For about 10 percent of the population, that was as early as their 20s. By age 50, as many as 50 percent of the population show signs.2
Other research shed more light on the issue and showed that we start losing brain function as early as our 40s.3
Hope comes in the form of those who don’t suffer from the disease. Like the 115-year-old woman researchers studied after she died from stomach cancer. They learned from her that brain disease is not inevitable. They concluded, “The limits of human cognitive function extend far beyond the range that is currently enjoyed by most individuals; brain disease, even in supercentanarians, is not inevitable.”4
The key is to make changes today. If you wait to see if you will suffer from these issues, it could be too late. A cure may be impossible, because Alzheimer’s fatally damages neuronal networks. Dead nerve cells cannot be brought back to life.
One of the key factors in the development and progression of Alzheimer’s dementia, may be a lack of adequate blood flow to the brain due to clogging of cerebral arteries. This clogging is otherwise known as atherosclerosis.
We usually associate atherosclerosis with the heart, but it involves every part of the human vascular tree. This means there is a link among coronary artery disease, degenerative brain disease and dementia. In fact, a substantial body of evidence strongly associates atherosclerosis—or this clogging of the arteries—with Alzheimer’s disease.
I take that as good news because heart disease is preventable and reversible in most cases through diet and other lifestyle changes. More research needs to be done to know if the same is true of Alzheimer’s, but research available today seems to indicate that is the case.
A 2009 study in the journal Neurology showed that in 300 patients with Alzheimer’s, “treatment of vascular risk factors [was] associated with a slower decline” of their disease than those who went untreated.5
Other research showed that study “participants with moderate or severe intracranial arterial stenosis had a faster decline in cognition and function relative to participants without such stenosis.”6 Intracranial arterial stenosis is when a brain artery (or arteries) get narrower.
Combined, these studies indicate that when we treat the risk factors for developing vascular disease overall, we can at least slow down progression to Alzheimer’s. This means that if you don’t have the disease today, you can slow down the possibility of manifesting it later, even if you’re brain is already heading in that direction.
So how do you do that? How do you minimize your risk of developing any type of vascular disease whether it’s heart disease, or Alzheimer’s or other forms of dementia? Lifestyle changes.
If you’d rather die than eat more vegetables, consider Evelyn Oswick, one of the stars of the Forks Over Knives documentary. In her 50s, Evelyn suffered two heart attacks. She had an angioplasty and a triple bypass.
Then her cardiologist told her there was nothing more medicine could do for her so he suggested she join a research study at the Cleveland Clinic, run by Dr. Caldwell Esselstyn. The study looked at whether a whole-food, plant-based diet would help people with severe cardiac problems. People who were enrolled in the study were all told there was no other recourse.
When Dr. Esselstyn first told Evelyn about the study, she said would rather die than be on his program.
Evelyn did die. But only after she lived to be 90 years old, more than 30 years after she was told she would die young.
The thing is, she reconsidered her decision about joining the study. In a recorded interview when she was in her 80s, she said, “I’m very happy to be healthy, and have a lot of fun in life.”
This is the same woman who was told she wouldn’t live out the year more than 20 years previously. Who knows how long she would have lived if she had not joined the whole-food, plant-based lifestyle program? However, it was clear that if she lived in her former condition, her life would have been a string of doctor visits and poor health.
When it comes to Alzheimer’s, the research seems to indicate that we all have the same choice Evelyn did with her heart disease. There are many dietary changes that can help, starting with those that already have been shown to help repair and reverse heart disease.
Helpful dietary changes includes significantly reducing fat, especially saturated fat, and choosing a wide variety of greens, vegetables, fruits and whole grains over meat and other animal products such as dairy and eggs. Animal fat has been linked to dementia. Researchers have studied individual foods, as well, such as berries and turmeric, with good results on cognitive decline, but eating a diet rich in a variety of plant-based nutrients is the best starting point.
Studies have shown that exercise helps, too. In a study of 33 adults, who ranged in age from 55 to 85 years old and who had mild cognitive impairment, researchers demonstrated that cognitive decline reversed through exercise. Drugs can’t do that.”7
The current available research indicates that the answer to Alzheimer’s disease lies in prevention through a person’s choice to exercise and eat a more whole-food, plant-based diet. For those who choose that route, there appears to be hope.
References
1. https://en.wikipedia.org/wiki/Alzheimer’s_disease
2. Neurobiol Aging. 1997 Jul-Aug;18(4):351-7.
3. Neurobiol Aging. 2005 Mar;26(3):335-40.
4. Neurobiol Aging. 2008 Aug;29(8):1127-32. doi: 10.1016/j.neurobiolaging.2008.04.010. Epub 2008 Jun 4.
5. Neurology. 2009 Sep 1;73(9):674-80. doi: 10.1212/WNL.0b013e3181b59bf3.
6. Neurology. 2014 Mar 11;82(10):842-9. doi: 10.1212/WNL.0000000000000185. Epub 2014 Jan 31.
7. Arch Neurol. 2010 Jan;67(1):71-9. doi: 10.1001/archneurol.2009.307.


Small change, big difference
Marianne* signed up for the 10-week WholeBlue Eating course during the last enrollment period. Although I have not designed the course to focus on weight loss, she decided her goal was to get thinner.
Because she doesn’t read English she found it difficult to navigate through the site and asked me instead to give her some tips so she could change her diet. I answered her with a question. “What do you eat for breakfast?”
She delivered her response with a laugh. “A lot of meat, bread and candy.” Then, her voice lowered, the twinkle in her eye disappeared, and she said, “You will probably make me give it all up.”
I asked another question. “Do you like fruit?”
Marianne’s response was emphatic. “I love fruit. I eat a lot of it, usually at night. But I don’t think it’s good for me.”
Her response is all too typical. Many people believe that fruit is not good for us. But fruit is one of the best things we can eat. Here are five research-based fruit facts that show that truth.
- Natural sugars from fruits and starchy root vegetables are nutritional powerhouses. They “come prepackaged with five classes of micronutrients, including water, antioxidants, vitamins, fiber and minerals” and help to keep blood glucose in the normal range.1
- Foods containing manmade, refined sugars like sucrose, dextrose, high-fructose corn syrup and maltodextrin do spike blood glucose.1
- Several key nutrients in vegetables, fruits and beans are associated with better bone mineral density.2
- “Those eating fruits and vegetables each day have a higher likelihood of being classified as ‘very happy,’ suggesting a strong and positive correlation between fruit and vegetable consumption and happiness, perhaps feelings of optimism, too.”3
- A study published in Metabolism, put people on a 20-servings-of-fruit-a-day diet for a few weeks and found “that very high-vegetable fiber intakes reduce risk factors for cardiovascular disease and possibly colon cancer.”4
Knowing this research and more, my advice for Marianne was to replace the candy with whole fruit, and keep the bread, as long it was 100 percent whole grain. I added one thing she didn’t like hearing. “You will have to give up the meat.”
“I need the meat or I get hungry an hour or two later.”
I know how she felt. When I ate a diet heavy in animal-based proteins, I had the same problem. I explained to her she could put nut butter on the bread or she could replace the meat with a whole grain cereal and some nuts. I re-emphasized that she should eat as much fruit as she wanted for breakfast. She looked skeptical.
I also explained that whatever she chose, whenever she replaced animal-based proteins she should eat more quantity, though it may hard to believe one can eat more and still lose weight. She liked the sound of that.
Six weeks later Marianne and I met again. Her face was glowing. She was very excited. “I did what you said. I now eat cooked cornmeal (polenta) for breakfast with a plant-based milk and lots of fruit. I love it so much! And look, I can finally fit into these pants that I couldn’t fit into for many months.”
I think I was as surprised as she was. I didn’t think one small change a day could have such a dramatic effect. However, we both saw that it did.
What one thing can you do today toward a stronger, more whole you?
If you want to put your name on the waiting list for the next WholeBlue Eating course so you can join a community of people making small changes like Marianne made and more, please go to the course site and add your name to the waiting list.
*Not her real name.
References
- Top 3 Diabetes Myths, Busted: Fruit, Starchy Vegetables, and Blood Glucose. Cyrus Khambatta, PhD.
- Am J Clin Nutr. 2000 Jan;71(1):142-51
- NutritionFacts.org
- Metabolism. 2001 Apr;50(4):494-503.
May 22, 2017 News from WholeBlue Eating
Help and hope for achy joints
Arthritis is the No. 1 cause of disability in the United States, with more than 50 million people suffering some form of this sometimes-crippling disease. The bad news is experts at the Arthritis Foundation expect these numbers to keep growing.1 The good news is that some recent research results have shown promise in alleviating symptoms in many sufferers.
The term arthritis actually refers to joint pain or joint disease, comprising more than 100 different types of conditions. No age, sex or race is immune to all of the forms of arthritis; however, it is more common among women and tends to occur more frequently as people age.
Arthritis is often categorized into four types: degenerative, inflammatory or autoimmune, infectious, and metabolic.
Degenerative arthritis
The most common type of arthritis is degenerative osteoarthritis. This occurs when cartilage—the cushioning surface within bones—wears away. When this happens, pain, swelling, and stiffness come from bone rubbing against bone. As joints lose strength over time, pain can become chronic.
Inflammatory (or autoimmune) arthritis
Inflammatory arthritis comes when a person’s immune system attacks the joints with inflammation. The body mistakenly believes there is an invading substance and is just doing its job to protect. However, this mistaken attack can cause joint erosion and damage internal organs, eyes and other parts of the body. Smoking can trigger rheumatoid arthritis in people with certain genes.
Infectious arthritis
Another way a person can get arthritis is through a bacterium, virus or fungus that enters the joints and triggers inflammation. These invaders can include salmonella, food poisoning or contamination, sexually transmitted diseases, and hepatitis C. This form of arthritis, if caught in time, can often be successfully treated with antibiotics.
Gout (or metabolic arthritis)
The final type, metabolic arthritis, or gout, can occur in people who have too much uric acid in their bodies. Normally, uric acid is formed as the body breaks down purines, found in our cells naturally as well as in many foods. However, some people have more uric acid than they can get rid of. This buildup can cause needle-like crystals in the joint, resulting in sudden spikes of extreme joint pain. For some people, these arthritic or gout attacks are episodic. For others, the pain becomes chronic, with ongoing disability.
What can be done?
Treatment options vary with the type of arthritis. They include medications, surgery and natural alternatives such as herbs and supplements, exercise, massage, mind-body therapy, aromatherapy, electrical stimulation and diet. The type of treatment that works for a sufferer depends on the form of arthritis as well as the person.
For example, osteoarthritis can be prevented by staying active, maintaining a healthy weight, and avoiding injury and repetitive movements. Gout can be treated with medicines to reduce the uric acid levels in the body.
There is one treatment option that appears to help reduce the painful symptoms of all types of arthritis. Diet.
This option is not (just) about losing weight, it’s about eating the foods that help to reduce or eliminate the symptoms of arthritis.
Here are just a few examples:
- Reduce sodium. Research has shown that salt appears to drive autoimmune disease. Other research shows that a high-salt diet can overwork the kidneys, starving them of oxygen, which triggers inflammation.2
- Add sesame seeds. One research study looked at what happened when patients with osteoarthritis of the knee were given a quarter-cup of sesame seeds a day for two months, compared with patients with no sesame seeds. Both were given the standard treatment for their disease. While the placebo effect can’t be ruled out in this study due to its design, the pain in the sesame group dropped significantly lower than the control group.3
- Include turmeric in your diet. The effectiveness of curcumin on joint pain was first demonstrated more than 30 years ago. Interestingly, the drug it was compared to in that double-blind crossover study, phenylbutazone, was pulled from the market three years after the study because some people died from it.4 More recently, 45 patients diagnosed with rheumatoid arthritis were randomized into three groups: curcumin, the standard-of-care drug, or both. The curcumin groups showed significantly more improvement than those in the drug group. This means that curcumin was more effective in alleviating pain than the leading drug of choice, without any apparent adverse side effects.5
- Eat potassium-rich foods. While potassium is commonly known to lower blood pressure and stroke risk, a randomized, double-blind, placebo-controlled trial of potassium supplementation was tried in patients with rheumatoid arthritis. Published in 2008 in the official journal of the American Pain Society, the study found that potassium helped lower pain.6 The best news is you can eat those foods today. The six foods highest in potassium include: beans, especially white beans; dark leafy greens, especially spinach; baked potatoes with the skin; dried apricots; and baked acorn squash. Other great sources of the mineral include avocados, mushrooms and, of course, bananas.
- Eat a whole-food, plant-based diet. We have known this for a long time, but medical professionals often omit advice to do so, in large part because this is not emphasized in medical school. A study demonstrating the beneficial effect of a plant-based diet was published nearly 20 years ago.7 There have been other studies since.
- Don’t stay way from the purine-rich foods. Meat and seafood can trigger gout. Sufferers are often told to stay away from these foods, as well as mushrooms, peas, beans, lentils, and cauliflower. However, a study in the New England Journal of Medicine found that while sufferers are wise to stay away from meat and fish, the plant-based foods were actually found to be protective.8
While there are no guarantees that a diet will help all of your pain and other symptoms, there is compelling evidence that it should help some for most people. The best part is that a whole-food, plant-based diet comes without side effects, so eat away. However, if you want to make any changes to your medication routine given the results of your dietary changes, please do so only under the guidance of qualified medical care.
References
1. Arthritis Foundation
2. Nature. 2013 Apr 25;496(7446):518-22. doi: 10.1038/nature11868. Epub 2013 Mar 6.
3. Int J Rheum Dis. 2013 Oct;16(5):578-82. doi: 10.1111/1756-185X.12133. Epub 2013 Jun 20.
4. Indian J Med Res. 1980 Apr;71:632-4.
5. Phytother Res. 2012 Nov;26(11):1719-25. doi: 10.1002/ptr.4639. Epub 2012 Mar 9.
6. J Pain. 2008 Aug;9(8):722-31. doi: 10.1016/j.jpain.2008.03.006. Epub 2008 May 12.
7. Am J Clin Nutr. 1999 Sep;70(3 Suppl):594S-600S.
8. N Engl J Med. 2004 Mar 11;350(11):1093-103.

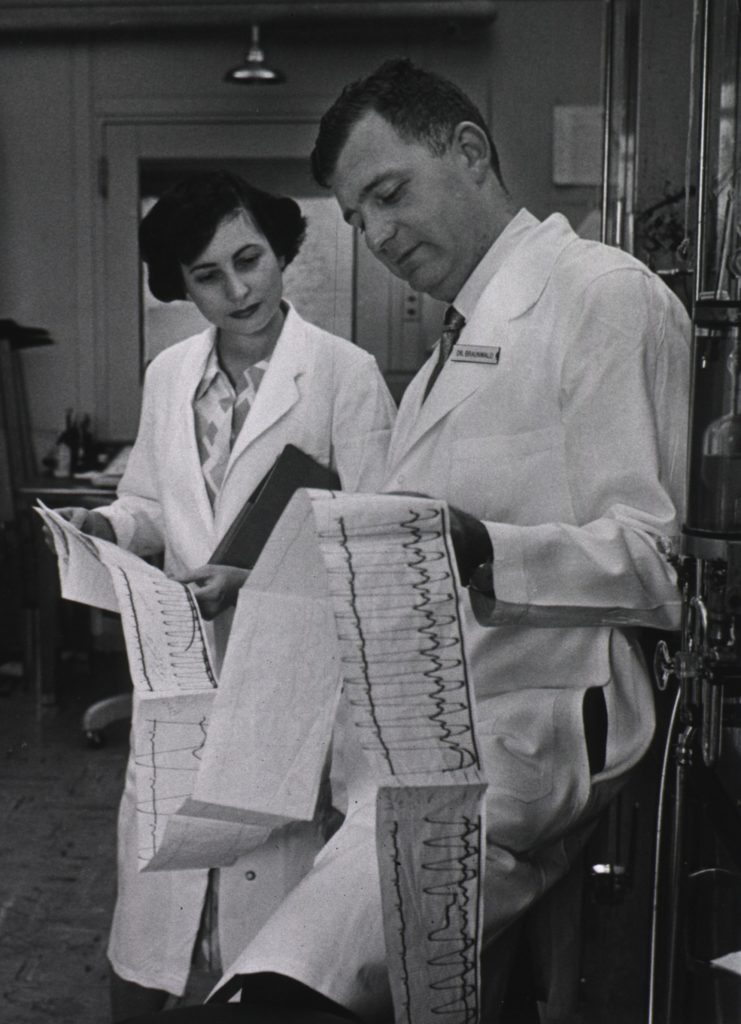
Striking strokes
When my dad went into the hospital for an aortic valve replacement, we all expected the surgery to make him feel better. He was first told he would someday need the surgery to correct this congenital condition back when he was in his 50s. It had been 20 years. The surgery was necessary.
After the late-day procedure, which went well, we left him in the recovery room with a promise to return early the next day. He was still groggy from the anesthesia.
When I entered his room the next morning, he was propped in bed struggling to get a spoonful of cereal. He looked at me. The side of his face was droopy and smeared with oatmeal. After spending a few more minutes with him, helping him to eat, I saw he had suffered a stroke.
I am not a trained medical professional, but I worked with a neurologist, and had seen stroke patients before. His symptoms were classic.
I used to think his stroke had a lot to do with his surgery, and it certainly played a role, but I now understand that his nearly clogged arteries played an even greater role. We often hear how high cholesterol leads to heart disease, but we rarely hear of its role in stroke and dementia, which are equally devastating when they strike.1
While there are three types of strokes, the most common are ischemic strokes, occurring in about 87 percent of stroke patients.2 This type of stroke happens when the artery that supplies oxygen-rich blood to the brain becomes blocked.
The second type, a hemorrhagic stroke, happens when an artery in the brain leaks blood or breaks open. The leaked blood puts pressure on the brain cells, damaging them. The third type, transient ischemic attacks (TIA) are also sometimes called “mini-strokes.” These are different from the major types only because blood flow is blocked for just a short time—usually less than 5 minutes.3
Regardless of the type, stroke kills. One out of every 20 deaths is due to stroke. In fact, every four minutes, someone in the United States dies of stroke. For those who survive, stroke leads to disability. In fact, it is the leading cause of serious long-term disability.
Although my dad’s stroke was relatively minor, the disability he suffered began his eight-year decline into death. I used to believe that this sort of decline is inevitable.
High blood pressure, high cholesterol and smoking are the leading causes of stroke.4 For me, the only preventable piece of that was the smoking, but I never smoked. I figured I was doomed with my genetic predisposition to high blood pressure and high cholesterol—things both my parents suffered.
It was only recently that I learned that not only are up to 80 percent of strokes avoidable with simple lifestyle changes, but those changes aren’t to just quit smoking. There are a few things everyone can do immediately to start decreasing their risk of stroke and other vascular diseases.
The first is to start eating more whole foods. Several studies have demonstrated the relationship between decreased stroke and other diseases and increased consumption of whole plant foods. One study published in a 2015 issue of BMC Medicine noted that “consumption of whole grains and cereal fiber was inversely associated with reduced total and cause-specific mortality. Our data suggest cereal fiber is one potentially protective component.”5
A study in a 2008 issue of Circulation found similar results. “A low-risk lifestyle that is associated with a reduced risk of multiple chronic diseases also may be beneficial in the prevention of stroke, especially ischemic stroke.”6 Their parameters defined a low-risk lifestyle as including a healthy diet, that is, more fruits, vegetables and whole grains.
Another helpful dietary change is to decrease refined sugar consumption. According to an article in the Journal of the American Medical Association, the “overconsumption of added sugar has long been associated with an increased risk of cardiovascular disease.”7
Soda drinkers must keep in mind that soda is a huge source of sugar, with as much as 6 tablespoons of processed sweetener in each 12-ounce can. Diet soda isn’t any better for cardiovascular risk. “Routine consumption of diet soft drinks is [associated with] increases in the same risks that many seek to avoid by using artificial sweeteners—namely type 2 diabetes, metabolic syndrome, heart disease and stroke.”8
Calcium supplementation can also lead to increased vascular disease. According to an article in the British Medical Journal, “calcium supplements with or without vitamin D modestly increase the risk of cardiovascular events, especially myocardial infarction.”*9
And if you’ve heard that fish oil can help protect you against stroke, consider these recent studies. A systematic review and meta-analysis published in the Journal of the American Medical Association evaluated the best randomized clinical trials looking at the effects of omega-3s on lifespan, cardiac death, sudden death, heart attack and stroke. Researchers found that consumption of fish oil or oily fish was “not associated with a lower risk of all-cause mortality, cardiac death, sudden death, myocardial infarction, or stroke based on relative and absolute measures of association.”10
Another review, published in the Annals of Internal Medicine, found that “omega-3 polyunsaturated fatty acid supplements do not reduce major cardiovascular events in adults.”11
There is so much more, but for now, these are some of the more important and easiest shifts you can make so that the only stroke in your future is a stroke of good luck.
_____________________________
*Please consult a qualified health professional before making changes to any prescribed medications or supplements.
References
- Cholesterol & Alzheimer’s Disease. Michael Greger M.D. FACLM October 9th, 2015 Volume 27.
- Mozzafarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al., on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation 2016;133(4):e38–360.
- American Heart Association/American Stroke Association. TIA (Transient Ischemic Attack). Accessed May 19, 2017.
- Berry JD, Dyer A, Cai X, Garside DB, Ning H, Thomas A, et al. Lifetime risks of cardiovascular disease. N Engl J Med 2012;366:321–9.
- BMC Med. 2015 Mar 24;13:59. doi: 10.1186/s12916-015-0294-7.
- Circulation. 2008 Aug 26;118(9):947-54. doi: 10.1161/CIRCULATIONAHA.108.781062. Epub 2008 Aug 12.
- JAMA. 2009 Oct 28;302(16):1741-2. doi: 10.1001/jama.2009.1534.
- Behav Anal. 2015 Mar 12;38(1):1-17. doi: 10.1007/s40614-015-0028-3. eCollection 2015 May.
- BMJ. 2011 Apr 19;342:d2040. doi: 10.1136/bmj.d2040.
- JAMA. 2012 Sep 12;308(10):1024-33. doi: 10.1001/2012.jama.11374.
- Ann Intern Med. 2012 Dec 18;157(12):JC6-5. doi:10.7326/0003-4819-157-12-201212180-02005.
April 24, 2017 News from WholeBlue Eating
I’ll Pass. I never get the flu.
When I worked in healthcare quality improvement, one of my tasks was to help physicians increase the number of patients who received an annual immunization for influenza.
One of the doctors I worked with, who had recently moved to Colorado from Illinois, asked me an interesting question. “Why do so many people in Colorado ignore my recommendations to get a flu shot?” She went on to tell me that such questioning of doctor’s recommendations was rare in the Midwest.
It’s a good question. Most people decline a vaccine because they believe the risk of the disease is less than the risk of the vaccine. For example, in 1955, “inadvertent inclusion of live polio vaccine in the killed Salk vaccine resulted in 40,000 cases of abortive (transient) polio, 51 cases of paralytic polio, and 5 deaths.”1
That particular case was tragic, and that particular vaccine was immediately discontinued. The polio vaccine used after that also had risk, where “roughly 4 or 5 children in the United States per year would acquire vaccine-associated paralytic polio.” However, that risk was “felt to be acceptable based on the superiority of the live vaccine in that it provided greater herd immunity.” It was also more cost effective, easier to administer and reduced transmission of the disease.
If you’re the parent of one of those children who acquired vaccine-associated polio, it would be heartbreaking. However, consider this. In the late 1950s more than 16,000 children died annually of the natural disease.
During the 1950s other diseases like whooping cough, polio, measle, and rubella struck hundreds of thousands of infants, children and adults in the United States, killing thousands every year.
As vaccines were developed and used, these diseases declined. For example, an epidemic of rubella in 1964–65 infected 12.5 million Americans, killed 2,000 babies and caused 11,000 miscarriages. Since 2012, 15 cases of rubella were reported to CDC.
Another example comes with diphtheria. In 1921, more than 15,000 Americans died from this disease, before there was a vaccine. Compare that to only two cases reported to the Centers for Disease Control between 2004 and 2014.2 Today that is the case for many diseases thanks to vaccinations.
So, does that mean we no longer need to vaccinate our children?
No. It means we are doing a good job and need to keep it up. Because if one or two cases of one of these now-rare diseases are introduced into a community, where most people are not vaccinated, outbreaks will occur.
For example, several measles outbreaks occurred around the country in 2013, including large outbreaks in New York City and Texas. These were areas that had low vaccination rates. If every community drops to low vaccination levels we could see a recurrence of some of these currently uncommon diseases.3
While we have very low rates of vaccine-preventable diseases in the United States, this isn’t the case globally. With easy travel, a resurgence of a vaccine-preventable disease is just a plane ride away.
As an adult, one vaccine you should still be getting is the flu vaccine. I’ve heard many of the common arguments against it, such as, “I got that once but it gave me the flu.” Or, “It doesn’t work.” But we just don’t know how good we have it.
Between 1918 and 1919, before the discovery of the influenza vaccine, approximately one-third of the world’s population (or 500 million people) were infected and had clinically apparent influenza.4 Total deaths from the flu worldwide were estimated between 50 million and 100 million.
According to a Stanford University web page devoted to this epidemic, “more people died of influenza in a single year than in four years of the Black Death Bubonic Plague from 1347 to 1351. Known as the ‘Spanish Flu’ or ‘La Grippe,’ the influenza of 1918-1919 was a global disaster.”5
According to historians and epidemiologists, its cause was due in part to the soldiers living in brutal conditions in the trenches and unable to fight off illness. In addition, because of the war, many more people traveled between countries.
One of the startling characteristics of that epidemic was that it was most deadly for people who were between the ages of 20 and 40, generally the least likely to get sick with the flu. Yet approximately 43,000 active World War I servicemen died of the disease.
So, while even those facts won’t be enough to persuade some to get the flu vaccine, we should all at least be thankful for the disease-less world our ancestors have left for us, and that we don’t have to suffer the loss of loved ones at the hand of mysterious killers.
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3096324/
- https://www.cdc.gov/vaccines/vac-gen/whatifstop.htm
- American Academy of Pediatrics Committee on Infectious Diseases. Prevention of varicella: recommendations for use of varicella vaccines in children, including a recommendation for a routine 2-dose varicella immunization schedule. Pediatrics. 2007;120:221–231.
- https://wwwnc.cdc.gov/eid/article/12/1/05-0979_article
- https://virus.stanford.edu/uda/


You going to eat that?
Have you ever eaten an entire pint of ice cream because you were feeling depressed? Or sat in front of the television mindlessly changing channels and the next thing you knew the brand-new family-size bag of chips on your lap was empty?
If you do this with some regularity, you are likely an “emotional eater.”
According to medical author Roxanne Dryden-Edwards, MD, “Emotional eating is the tendency of its sufferers to respond to stress by eating, even when not hungry, often high-calorie or high-carbohydrate foods that have minimal nutritional value.”
Emotional eaters tend to crave “comfort foods,” like ice cream, cookies, chocolate, fries, chips and pizza. An equal number of people eat more when stressed, as eat less while stressed, about 40 percent, Dryden-Edwards said.
Emotional eating can be symptomatic of a form of depression. Yet most people who consume more food in response to stress or boredom (the two most common emotional eating triggers) do not have any other mental health issues, including depression.
The difference between emotional eating and disorders such as bulimia or anorexia has to do with the degree to which a sufferer engages in the activity. While the consequences of bulimia or anorexia can be life threatening, the consequences of emotional eating can include guilt for the over-eating episode, nausea and weight-related health problems including diabetes, high blood pressure, fatigue and high cholesterol.
Eating Disorder Hope, a U.S. organization formed in 2005 to offer hope, information and resources to individual eating disorder sufferers, notes that left unchecked, emotional eating can also lead to more problems. “Emotional eating … can, however, play a role in the development of serious eating disorders like Binge Eating Disorder and Bulimia nervosa.”
Just like the more serious eating disorders, emotional eating is a way to alleviate an emotional difficulty. Natasha Files, a social worker and counselor who specializes in eating disorders says, “Eating disorders, like substance abuse, become a means of attempting to manage emotional pain.”
The good news is, as with all eating disorders, there is help. Those who struggle with emotional eating may even be able to help themselves. Everyday Health offers additional insight and five tips to stop the cycle.
- Become a mindful eater.
- Build impulse control through practice.
- Use your nondominant hand to eat.
- Cool off cravings.
- Practice deep breathing.
For those who struggle with breaking free on their own, many counselors specialize in helping with eating disorders. Some people also see relief through energy psychotherapy, like Splankna.
Regardless of the option you choose to break free of this binding cycle, you’ll help yourself become stronger if you choose one today.
April 13, 2017 News from WholeBlue Eating
Are carbohydrates evil?
What the science says
I’ve been browsing recipes lately and came across a low-carbohydrate meal plan put out by a major health organization. It looks much like the plan recommended to me when I was prediabetic, but compared to what the science says, it seems the authors of the meal plan got a few things wrong.
It is common for people to believe that carbohydrates are bad for them. This is particularly true for people who are looking to lose weight, people who have diabetes or people who want to build muscle. Who hasn’t heard someone say, “I shouldn’t eat that potato. I’m trying to lose weight.”
For diets like the Atkins diet, many diabetic diets, or even the Paleo diet, the focus is put on protein instead of carbs. When these advocates do talk about carbohydrates, or carbs, they talk about “good” vs. “bad” carbs.
The scientific evidence supports the notion of good vs. bad when it comes to carbohydrates.
With their main purpose being to provide energy, carbohydrates are one of three macro nutrients key to optimal health (the other two are protein and fat). Carb molecules contain carbon, hydrogen and oxygen atoms. The group can be split into three categories: sugar, starches and fiber; however, most carbs are eventually broken into glucose to be used as energy. The exception to this is fiber, which helps to feed the friendly bacteria in the gut.
Described like that, carbs sound good. Who doesn’t need more energy?
The problem comes when we eat carbohydrates that don’t come with a lot of fiber. Such carbs give bodies a huge rush of energy and then leave them in the lurch. They include all refined grains like white rice and processed cereals; white flour and things made from it; nearly all sugars (including honey) and things made from them. They can also include whole foods like white potatoes.
This type of sugar rush is potentially troublesome for people with diabetic or prediabetic conditions, and is the reason they are often told to eat low-carbohydrate diets. Such recommendations can be fierce, even though the American Diabetes Association (ADA) itself makes no such recommendations. According to an association spokesperson, “There is no ADA diet and that the amount of carbohydrate, fat, and protein in the diet should be adjusted to meet treatment goals, as well as the patient’s lifestyle.”
With a few exceptions, the primary problem is we tend to eat carbs out of context, that is, we pull them out of the way nature made them. Things that are smooth and creamy and sweet sell. Rough, grainy and earthy things tend not to sell.
Whole carbs include vegetables, whole fruit, legumes and whole grains. Refined carbs include sugar-sweetened beverages, fruit juices, pastries and nearly any food with the word “white” in front of it like bread, pasta and rice.
Such whole carbs are very good for you, and the more plant-based the diet, the lower the rates of diabetes.1,2 In addition, beans, split peas, chickpeas and lentils may be the most important dietary predictor of survival.3 Low-carb diets that emphasize meat and animal proteins “impair arterial function, as evidenced by a decrease in flow-mediated dilation—meaning low-carb diets effectively cripple people’s arteries.”4 That is just one of the many deleterious effects of low-carb diets.
To complicate matters, manufacturers have learned to make food sound healthier so you see breads labeled “wheat bread” that just means it is made from wheat, still all or mostly white wheat. Or a label may say “made with whole grain,” but sugar and white flour are among the first three ingredients.
The only way you can be sure you are eating the healthiest carbs possible is to eat your carbs in context. Cook up some ground corn that includes the hulls, for breakfast. Eat brown, red or black rice instead of white. If you eat bread, eat bread made from a 100 percent whole grain like rye or wheat. Eat whole fruits and vegetables.
And when you eat potatoes, put a little color in your life.5 Purple potatoes can decrease inflammation, increase the antioxidant capacity of your bloodstream and help to lower blood pressure in people with hypertension.
If you want to live a long, healthier life, just don’t avoid the good carbs.
References
- Watzl B. Anti-inflammatory effects of plant-based foods and of their constituents. Int J Vitam Nutr Res. 2008 Dec; 78(6):293-8.
- S Tonstad, K Stewart, K Oda, M Batech, R P Herring, G E Fraser. Vegetarian diets and incidence of diabetes in the Adventist Health Study-2. Nutr Metab Cardiovasc Dis. 2013 Apr;23(4):292-9.
- I Darmadi-Blackberry, M L Wahlqvist, A Kouris-Blazos, B Steen, W Lukito, Y Horie, K Horie. Legumes: the most important dietary predictor of survival in older people of different ethnicities. Asia Pac J Clin Nutr. 2004;13(2):217-20.
- L. Schwingshackl, G. Hoffmann. Low-carbohydrate diets impair flow-mediated dilatation: Evidence from a systematic review and meta-analysis. Br. J. Nutr. 2013 110(5):969 – 970.
- Kaspar KL, Park JS, Brown CR, Mathison BD, Navarre DA, Chew BP. Pigmented Potato Consumption Alters Oxidative Stress and Inflammatory Damage in Men. J Nutr. 2011 Jan; 141(1):108-11.


Tastes like chicken
Many people turn to chicken as a protein source that is lower in fat than others. However, “there are a number of cuts of beef that have less cholesterol-raising saturated fat than chicken.”
Better yet, if you switch from meat to tofu, not only do you significantly lower fat intake but cholesterol goes down.1
People can lower their cholesterol 5 to 10 percent by cutting down on fatty meat, dairy and eggs, but you can lower cholesterol 10 to 15 percent on a vegetarian or flexitarian diet, 15 to 25 percent on a standard vegan diet, and up to 35 percent, in a matter of weeks, on a healthier plant-based diet.
So, if you have been advised to lower your cholesterol, consider your options for taking charge of your own health and lowering your cholesterol through diet, which has no side effects, instead of eventual medicines that often come with a host of side effects.
A great way to do this is to make things that “taste like chicken.”
Since going plant-based I have developed several recipes, including “No-chicken Chicken Soup” which a friend’s meat-eating husband insists she make regularly; No Chicken and Dumplings, and No Chicken Salad.* All are just as flavorful as their meaty counterparts (my husband thinks they are more flavorful) with many more health benefits.
What is your favorite plant-based recipe that “tastes like chicken”?
References
- E Ashton, M Ball. Effects of soy as tofu vs meat on lipoprotein concentrations. Eur J Clin Nutr. 2000 Jan;54(1):14-9. https://www.ncbi.nlm.nih.gov/pubmed/10694766
*All of the recipes mentioned in the newsletter and on the blog are available through the WholeBlue Eating course, which is offered up to three times a year. Click here to be put on the Wait List for the next course.
Sharing someone else's WholeBlue Newsletter? Sign up for the newsletter email list so you can get your own copy as soon as it comes out.
March 26, 2017 News from WholeBlue Eating
When Protein is Bad for You
Whether they know it or not, about one in eight Americans has chronic kidney disease (CKD). You may be at risk if you have high blood pressure or diabetes.
The National Institute of Diabetes and Digestive and Kidney Diseases tracks such statistics and notes that “the incidence of recognized CKD in people ages 65 and older more than doubled between 2000 and 2008.”
A primary risk factor for both diabetes and high blood pressure — the leading causes of CKD — can be summed up in one word: Meat.
A 2013 meta-analysis published in Current Diabetes Reports reviewed all the cohorts concerning meat and diabetes and found a higher risk associated with total meat consumption, especially processed meat. In addition, according to research summarized on NutritionFacts.org, “food of animal origin is highly significantly associated with [high] blood pressure.”
High animal protein intake, including meat, is also directly associated with kidney problems. As early as 1998, with a study published in Nephron, we’ve known that “animal protein intake has a profound effect on normal human kidney function … increasing the workload.”
By contrast, plant protein does not have the same effect, for both nondiabetics and diabetics with normal kidneys. In 2014, a six-month, double-blind, randomized, placebo-controlled trial published in Clinical Biochemistry compared the effects of animal proteins to plant protein on kidney function and found that “whole soy consumption tended to improve markers of renal function relative to control.” That is, things got better with soy.
If you have high blood pressure or diabetes, next time you visit your doctor ask if you’re being checked for kidney disease. In the meantime, this research indicates it would be good to add more plant-based protein in place of the animal protein in your diet.


Eat your Spinach and Laugh
It’s a happy coincidence that International Mirth Month (March) and National Spinach Day (March 26 this year) come in the same month or is it?
A 2012 study published in the journal Public Health Nutrition found that “more frequent consumption of vegetables seems to be protective against depressive symptoms” within two weeks. And a review in the journal Nutritional Neuroscience says that eating a lot of fruits and vegetables may present “a noninvasive, natural, and inexpensive therapeutic means to support a healthy brain.”
According to the U.S. National Institute of Mental Health, depression is common but serious. “It causes severe symptoms that affect how you feel, think, and handle daily activities, such as sleeping, eating, or working.”
Depression takes several forms. The five more common forms are:
- Persistent depressive disorder, a depressed mood that lasts for at least two years.
- Perinatal depression that many women experience after giving birth.
- Psychotic depression, which occurs when a person has severe depression plus some form of psychosis.
- Seasonal affective disorder, which begins during the winter months, when there is less natural sunlight.
- Bipolar disorder, which includes episodes of extremely low moods coupled with extreme highs.
What do you do if you’re feeling blue?
In addition to traditional forms of treatment for depression such as medications, exercise, and talk therapy, or a combination of treatments, some people have found relief through energy therapy. Dr. Ann Marie Chiasson, a family medicine doctor trained in integrative medicine who is also an energy healer, spoke of her experience treating several patients with a variety of ailments in an online article in Psychology Today, posted July 2, 2011.
Dr. Chiasson described depression, for example, as “a disconnection of the energy body from our physical body.” In her work with depression, she tries “to ‘ground’ a person’s energy lower in the body in order to heal the depression.”
Another tool that has shown effectiveness in depression is the Emotional Freedom Technique, or EFT. Ben Schwarcz says, on his website, “Since I’ve been using EFT for depression treatment with my psychotherapy clients, I’ve often cut the length of treatment dramatically.”
Many Splankna practitioners, have seen improvement in patients who have described depression symptoms as well. Splankna is a mind-body procedure for alleviating emotional trauma that includes some parts of EFT in its comprehensive protocol. More about the protocol is available here.
So if you’re feeling depressed, even mildly, think about what you can do to help your mood, whether it’s traditional counseling, a medical doctor, or an energy practitioner such as a Splankna practitioner. It is International Mirth Month, after all.
And eat (or drink) your greens (or smoothies). Not only could it help with your mental health, you could possibly live longer in your state of mirth. A 2009 study in Preventative Medicine notes that one of the six most powerful things we can do to live longer is to eat green leafy vegetables. Doing so may cut our risk of premature death by 20 percent to 25 percent.
If you need some ways to do so, check out the three simple recipes for spinach in this issue. You can find the recipes here.
Plant-based for health?
There’s some evidence that some vegetarians are experiencing more mental-health issues compared with meat-eaters. But most plant-based eaters live longer, mentally- and physically-healthier lives than others.
What’s the difference?
Many vegetarians and vegans eat plant-based, but for them that may mean beer, brownies, doughnuts, highly processed fake meats, and other unhealthy foods. A vegan or vegetarian diet that has a high percentage of “junk” food would show deficiencies. According to an article in Women’s Health magazine, healthy levels of zinc, B vitamins, and iron can be difficult for vegetarians to maintain.
However, vegetarians who eat a full complement of healthy beans, greens, fruits and vegetables every day and minimize processed and other junk foods typically don’t have this problem.
If you decide a plant-based diet is for you, make sure you go into it fully expecting to eat whole, plant-based foods, not junk or processed foods, to avoid these problems.
You will also need to supplement B12 and should consider taking Vitamin D (whether you’re plant-based or not). One other supplement to consider is a vegan form of DHA, such as algae. For some great science-based guidance on optimum nutrition recommendations, visit NutritionFacts.org.
Otherwise, your food is your medicine. Anything else you should probably discuss with your plant-based (or regular) doctor.
